Health
What Weight Loss Surgery is Best For the Body?
Last Updated on May 16, 2023 by Nurse Vicky
What Weight Loss Surgery is Best For the Body?
In today’s fast-paced world, weight loss has become a significant concern for many individuals. While various methods exist to shed excess pounds, weight loss surgery has gained prominence as an effective solution for individuals struggling with obesity.
This article aims to unravel the mystery surrounding weight loss surgeries and provide detailed information on the different types of surgeries available, their benefits, risks, and considerations to help you make an informed decision.
Understanding Weight Loss Surgeries and Their Purpose
Weight loss surgeries, also known as bariatric surgeries, are medical procedures designed to help individuals achieve significant and sustained weight loss by altering the digestive system.
These surgeries work by restricting the amount of food the stomach can hold or by limiting the absorption of nutrients. The primary purpose of weight loss surgeries is to improve overall health and reduce the risk of obesity-related health conditions, such as diabetes, high blood pressure, and heart disease. Different Types of Weight Loss Surgeries
Gastric Bypass Surgery
Gastric bypass surgery is one of the most common and effective weight loss procedures. During this surgery, the surgeon creates a small pouch at the top of the stomach and connex cts it directly to the middle portion of the small intestine, bypassing a significant portion of the stomach and upper small intestine. This results in reduced food intake and decreased nutrient absorption.
Sleeve Gastrectomy
Sleeve gastrectomy involves removing a large portion of the stomach, leaving behind a smaller sleeve-shaped stomach. This procedure restricts food intake by reducing the stomach’s size and removing the part responsible for producing hunger-inducing hormones.
Adjustable Gastric Banding
Adjustable gastric banding is a reversible weight loss surgery that involves placing an inflatable band around the upper part of the stomach, creating a small pouch. The band can be adjusted to control food intake by tightening or loosening it. This procedure does not involve any removal of stomach tissue.
Biliopancreatic Diversion with Duodenal Switch
This complex weight loss surgery involves removing a significant portion of the stomach and rerouting the small intestine to limit both food intake and nutrient absorption. It is usually recommended for individuals with a high body mass index (BMI). Factors to Consider Before Undergoing Weight Loss Surgery
Eligibility and Evaluation
Before undergoing weight loss surgery, individuals are evaluated by healthcare professionals to determine their eligibility. Factors such as BMI, medical history, previous weight loss attempts, and overall health are taken into account. It’s important to consult with a qualified surgeon to assess your suitability for surgery.
Potential Risks and Complications
Like any surgical procedure, weight loss surgeries carry risks. These may include infection, bleeding, blood clots, and adverse reactions to anesthesia. Additionally, long-term complications such as malnutrition, gallstones, and hernias may arise. Understanding the potential risks and complications is crucial in making an informed decision.
Lifestyle Changes and Commitment
Weight loss surgery is not a magic solution. It requires a commitment to significant lifestyle changes, including adopting a healthy and balanced diet, engaging in regular physical activity, and attending follow-up appointments. Patients must be willing to make these changes to achieve long-term success.
Benefits of Weight Loss Surgery
Significant and Sustained Weight Loss
Weight loss surgery has been proven to provide significant and sustained weight loss for individuals struggling with obesity. Many patients experience improvements in overall health, including reduced blood sugar levels, improved cholesterol profiles, and decreased blood pressure.
- Resolution of Obesity-related Health Conditions
- Weight loss surgery often leadsBenefits of Weight Loss Surgery (continued)
Resolution of Obesity-related Health Conditions
Weight loss surgery often leads to the resolution or improvement of obesity-related health conditions. Many individuals with type 2 diabetes, sleep apnea, and high blood pressure experience significant improvement or complete remission after undergoing weight loss surgery. This not only enhances their quality of life but also reduces the need for long-term medication.
Enhanced Mental and Emotional Well-being
Obesity can take a toll on an individual’s mental and emotional well-being, leading to low self-esteem, depression, and anxiety. Weight loss surgery can contribute to improved mental health by boosting self-confidence and body image. Patients often report increased energy levels, better moods, and an overall positive outlook on life.
Choosing the Best Weight Loss Surgery for You
When it comes to selecting the most suitable weight loss surgery, there is no one-size-fits-all approach. The decision should be based on individual factors, including medical history, current health conditions, weight loss goals, and the advice of a qualified healthcare professional. It is essential to have a thorough discussion with your healthcare team to determine which weight loss surgery option aligns best with your needs and preferences.
Factors to Consider When Choosing a Weight Loss Surgery
Weight Loss Goals and Expectations Consider your weight loss goals and expectations. Some weight loss surgeries may lead to more significant weight loss than others. Discuss your desired outcomes with your healthcare provider to ensure realistic expectations are set.
Health Conditions and Medical History
Evaluate your current health conditions and medical history. Certain weight loss surgeries may be more suitable for individuals with specific health concerns. It is important to disclose all relevant information to your healthcare team to make an informed decision.
Lifestyle and Commitment
Assess your lifestyle and commitment level. Different weight loss surgeries require varying degrees of lifestyle changes and long-term commitment. Understand the dietary and physical activity modifications necessary for each procedure and determine which one aligns with your ability to adopt and sustain those changes.
You may be wondering what type of weight loss surgery is best for your body. There are several different options to consider including Gastric bypass, Sleeve gastrectomy, Intragastric balloon, and Transarterial embolization.
The following article will help you choose which option is best for your body. You may also be interested in learning more about the pros and cons of each procedure. The following is a comparison of the two most common surgeries.
Gastric bypass
The Gastric Bypass is the best weight loss surgery for the body. It removes a large portion of the stomach and creates a small tube that holds the remaining contents. This surgery allows the body to feel full faster, as the stomach no longer contains as much food as it did before.
The surgery also improves insulin resistance, since the stomach no longer produces the hormone that triggers hunger. The surgery is permanent and cannot be reversed. The Roux-en-Y gastric bypass is the gold standard of weight loss surgery.
This procedure reduces the size of the upper stomach and limits the amount of food the body can absorb. The food bypasses the duodenum and the upper part of the small intestine. This helps reduce fat, calories, and the absorption of vitamins and minerals. Patients will lose a significant amount of weight, but their bodies will still be affected by the procedure.
Sleeve gastrectomy
If you’re overweight and not happy with your eating habits, Sleeve gastrectomy surgery may be the perfect option for you. The procedure involves cutting off the upper portion of the stomach, allowing you to eat less and maintain a healthy weight.
It can help you lose as much as 60% of your excess weight in just two years. A Sleeve gastrectomy will require regular medical checkups and dietary recommendations, but the results can be long-lasting. After the procedure, you will likely be released from the hospital after an hour or two.
In the days following surgery, you will be placed on a liquid diet, and you will gradually be allowed to eat small amounts of food. Following your recovery, you should avoid consuming large quantities of food for the first few days, as this can cause pain and discomfort.
The surgery is minimally invasive, and most patients can return to work within one to two weeks, although you will need to modify your activities for the first few weeks.
The first question that may arise in your mind is whether an intragastric balloon is the right weight loss surgery for you. If you have undergone bariatric surgery before, this procedure may not be right for you.
It can also affect your health if you have an inflammatory bowel disease. Other disqualifying factors for the surgery include a gastric mass or a hiatal hernia.
Intragastric balloon weight loss surgery results in an average loss of 60 to 70 percent of body weight, which has a positive impact on obesity-related diseases.
Patients undergoing gastric balloon surgery usually lose about 10 to 15 percent of their body weight during the first six months after the procedure. However, the results are not as dramatic as with gastric sleeve surgery.
Furthermore, you must commit to a 12-month exercise and diet program after the surgery. You may also be required to undergo a behavioral therapy program to enhance your weight loss.
Transarterial embolization
Transarterial embolization is an image-guided procedure that targets the endocrine function of the gastric fundus, a part of the gastric wall that is responsible for controlling appetite. This new method of weight loss surgery has seen promising preliminary results in adults suffering from severe obesity.
It reduces excess body weight by up to 11% and causes up to 7.6 kilograms of weight loss in 20 patients. In the initial phase of the study, eight participants had minor adverse events. The ideal agent for LGAE is unclear, but it does reduce the options for established surgical bariatric procedures.
For example, volume reduction in the devascularised area of the stomach may be ineffective, and in some cases, surgery might be ruled out altogether. In some cases, a gastric banding procedure may be the only option for those patients who have failed to lose weight despite multiple attempts that have proven unsuccessful.
Transarterial sleeve gastrectomy
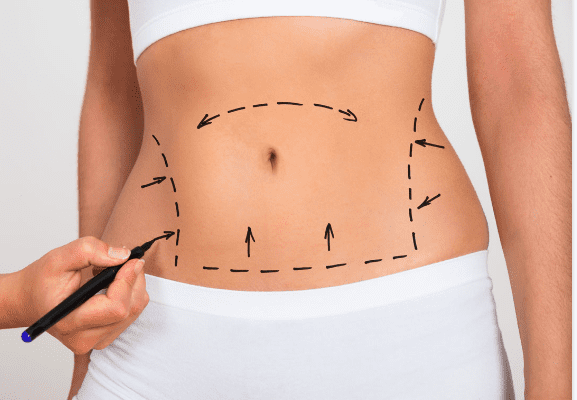
A sleeve gastrectomy is a surgical procedure that involves the removal of a portion of the stomach. The surgeon creates a narrow sleeve in the stomach by vertically stapling the abdominal wall and removing the larger, curved part of the stomach.
The procedure can take one to two hours. After undergoing surgery, patients typically spend one to two nights in a hospital. Afterward, they are awakened in a recovery room. A doctor will place small surgical tools, including a laparoscope, through a series of tiny incisions in the upper abdomen.
A sleeve gastrectomy is a surgical procedure that reduces weight by removing part of the stomach. By removing part of the stomach, the amount of ghrelin, also known as the “hunger hormone,” will decrease.
The patient’s insulin level will likely decrease immediately and they may no longer require medications to control their diabetes. While the procedure is generally safe, there are potential risks and complications.
Frequently Asked Questions
1 How long does it take to recover from weight loss surgery?
Recovery time can vary depending on the type of weight loss surgery. Generally, patients can expect a recovery period of several weeks before resuming normal activities.
2 Will I have to follow a specific diet after weight loss surgery?
Yes, dietary changes are a crucial aspect of successful weight loss surgery. Your healthcare team will provide you with a detailed post-surgery diet plan to follow.
2 Is weight loss surgery covered by insurance?
In some cases, weight loss surgery may be covered by insurance if certain criteria are met. It is advisable to contact your insurance provider to understand your coverage options.
3 Can weight loss surgery be reversed?
While some weight loss surgeries are reversible, others are considered permanent. It is important to discuss the reversibility aspect with your healthcare provider before undergoing any procedure.
4 Will I need to take supplements after weight loss surgery?
Supplements may be recommended to ensure adequate nutrient intake after weight loss surgery. Your healthcare team will guide you on the specific supplements you may need.
5 Are there any age restrictions for weight loss surgery?
Age restrictions may vary depending on the type of weight loss surgery and individual circumstances. Your healthcare team will evaluate your overall health and determine if you are a suitable candidate for weight loss surgery.
6 Can I get pregnant after weight loss surgery?
Weight loss surgery can affect fertility, but it is possible to get pregnant after the procedure. It is important to discuss family planning with your healthcare provider and ensure proper nutrition and monitoring during pregnancy.
7 What are the potential risks of weight loss surgery?
Weight loss surgery carries risks, including infection, bleeding, blood clots, and complications related to anesthesia. Long-term risks may include nutritional deficiencies and the development of gallstones. Your healthcare team will discuss these risks with you before the surgery.
8 How long does it take to see results after weight loss surgery?
Weight loss results vary among individuals and depend on factors such as the type of surgery, adherence to dietary guidelines, and lifestyle changes. Some individuals may experience significant weight loss within the first few months, while others may have a more gradual progression.
9 Will I need to attend support groups after weight loss surgery?
Joining a support group can be beneficial for individuals who have undergone weight loss surgery. These groups provide a supportive environment to share experiences, exchange advice, and receive emotional support throughout the weight loss journey.
Remember, the decision to undergo weight loss surgery should be made after careful consideration and consultation with healthcare professionals. Each individual’s circumstances are unique, and what works for one person may not be the best option for another.
By understanding the different types of weight loss surgeries available, and the associated benefits, risks, and considerations, you can make an informed choice that aligns with your goals and promotes your overall well-being.
Conclusion
Weight loss surgery can be a life-changing solution for individuals struggling with obesity. By understanding the different types of weight loss surgeries available, their benefits, risks, and considerations, you can make an informed decision about the best option for your body. Remember to consult with a qualified healthcare professional who specializes in bariatric surgery to assess your eligibility, address any concerns, and guide you through the process.
Health
Protein-Infused Diet Coke: The Viral ‘Dirty Soda’ Trend Taking TikTok by Storm

Protein-Infused Diet Coke: The Viral ‘Dirty Soda’ Trend Taking TikTok by Storm
The rise of quirky, unconventional food and drink trends is a staple of social media, but one concoction that’s recently captured TikTok’s imagination is “Protein Diet Coke,” fondly referred to as a “dirty soda.”
Combining the classic fizz of Diet Coke with creamy protein shakes, this bizarre yet fascinating combination has gained traction for its unique taste, nutritional benefits, and shareable aesthetic appeal.
But is it more than just a passing fad? Let’s dive into why this drink has taken the internet by storm, the health implications, and how you can make your own.
What Is Protein Diet Coke?
Protein Diet Coke is a mashup of two popular beverages: Diet Coke, known for its zero-calorie allure, and protein shakes, a go-to choice for fitness enthusiasts.
By blending these seemingly unrelated drinks, you get a fizzy, creamy concoction that surprises the palate and offers a protein-packed twist.
This beverage has become a TikTok sensation, with videos showcasing creative ways to personalize the drink by experimenting with flavors, toppings, and presentation.
How Did Protein Diet Coke Become a Trend?
The trend began with users sharing videos of themselves trying the drink and reacting to its surprising taste.
The hashtag #ProteinDietCoke amassed millions of views as influencers and everyday users alike showcased their custom recipes. Social media thrives on novelty, and the odd pairing of soda and protein shake fits the bill perfectly.
Moreover, this trend reflects a broader shift toward incorporating fun into fitness and healthy eating. As people explore unique ways to stay healthy, Protein Diet Coke offers a mix of indulgence and nutrition.
Health Benefits of Protein Diet Coke
1. Boosts Protein Intake:
Protein is essential for muscle repair, weight management, and overall body function. By mixing Diet Coke with a protein shake, you create a delicious way to meet your daily protein goals.
2. Low-Calorie Alternative:
For those watching their calorie intake, using Diet Coke and low-sugar protein shakes keeps the drink guilt-free while satisfying cravings for something sweet and fizzy.
3. A Fun Recovery Drink:
The combination of carbonation and protein makes this drink a potential post-workout recovery option. While traditional recovery drinks are effective, Protein Diet Coke brings a fun twist to replenishing nutrients.
Possible Drawbacks of Protein Diet Coke
While this beverage has many enthusiasts, it’s not without its critics.
1. Artificial Sweeteners:
Diet Coke contains artificial sweeteners like aspartame, which some people prefer to avoid due to potential health concerns.
2. Unusual Flavor:
Not everyone loves the combination of cola and creamy textures. For some, it’s an acquired taste.
3. Limited Nutritional Value from Soda:
Though protein shakes provide nutrients, the soda itself doesn’t offer significant health benefits. Consuming it in moderation is key.
How to Make Protein Diet Coke at Home
Ingredients:
- 1 can of Diet Coke (12 oz)
- 1 scoop or 8 oz of your favorite protein shake (vanilla or caramel flavors work best)
- Ice cubes
- Optional: toppings like whipped cream, syrups, or fruit
Instructions:
- Fill a glass with ice cubes.
- Pour the Diet Coke into the glass, leaving some space for the protein shake.
- Slowly add the protein shake to the Diet Coke. Stir gently to combine.
- Customize with toppings or syrups if desired.
- Enjoy immediately!
Why Do People Love It?
The allure of Protein Diet Coke lies in its unexpected combination and social media appeal.
The drink’s unique flavor profile intrigues people, while its aesthetic presentation makes it Instagram-worthy.
Additionally, it’s a fun way to consume protein without feeling like you’re drinking a traditional shake.
Creative Variations of Protein Diet Coke
1. Mocha Protein Soda:
Add a chocolate-flavored protein shake for a mocha-inspired treat.
2. Tropical Twist:
Use coconut-flavored protein powder and garnish with pineapple slices.
3. Spicy Cola Blend:
Mix in a dash of cinnamon or chili powder for a bold kick.
4. Vanilla Caramel Float:
Top with a dollop of whipped cream and caramel drizzle for an indulgent dessert-like drink.
Is Protein Diet Coke Here to Stay?
Trends often fade as quickly as they emerge, but Protein Diet Coke might have staying power due to its flexibility and nutritional appeal. As long as social media continues to celebrate creativity in the kitchen, this quirky beverage is likely to remain a go-to option for adventurous foodies.
Conclusion
Protein Diet Coke is more than just a viral sensation; it’s a testament to how creativity can turn everyday ingredients into something extraordinary.
While it may not replace traditional sources of protein or be everyone’s cup of tea (or soda), it has undeniably carved out a niche in the world of health-conscious indulgence.
Whether you’re in it for the taste, the health benefits, or the TikTok-worthy moments, this “dirty soda” trend is worth a try.
FAQs
1. Can I use regular Coke instead of Diet Coke?
Yes, but keep in mind that regular Coke has significantly more sugar and calories, which might defeat the purpose of a low-calorie drink.
2. What type of protein shake works best?
Vanilla and caramel protein shakes are popular choices because they complement the flavor of cola. However, feel free to experiment with other flavors.
3. Is Protein Diet Coke suitable for kids?
While it’s not inherently harmful, the caffeine content in Diet Coke might not be suitable for children. Opt for caffeine-free soda if making this for kids.
4. Can I make a vegan version?
Absolutely! Use plant-based protein shakes and ensure the soda is vegan-friendly.
5. How often can I drink Protein Diet Coke?
Like any treat, moderation is key. Consuming it occasionally as part of a balanced diet is perfectly fine.
References
Health
STI Epidemic: Decline in New Syphilis and Gonorrhea Cases in the US, CDC Reports
Health
Dave Coulier Opens Up About His Battle with Stage 3 Non-Hodgkin’s Lymphoma

Dave Coulier Opens Up About His Battle with Stage 3 Non-Hodgkin’s Lymphoma
A Beloved Star Faces a Serious Diagnosis
Dave Coulier, best known for his role as Joey Gladstone on the iconic sitcom Full House, has revealed a deeply personal health challenge.
The comedian and actor recently announced his diagnosis of Stage 3 Non-Hodgkin’s Lymphoma, sparking widespread concern and support from fans worldwide.
Coulier’s bravery in sharing his journey sheds light on this complex form of cancer, its symptoms, treatment options, and the importance of early detection.
What is Non-Hodgkin’s Lymphoma?
Understanding the Disease
Non-Hodgkin’s Lymphoma (NHL) is a type of cancer that originates in the lymphatic system, which is an integral part of the body’s immune defense.
This form of lymphoma is distinct from Hodgkin’s lymphoma due to differences in the cancerous cells’ appearance and behavior.
- Lymphatic System’s Role: It helps fight infections and regulates fluid balance in the body.
- Lymphoma’s Impact: NHL occurs when lymphocytes (a type of white blood cell) grow uncontrollably, leading to tumors.
Dave Coulier’s Journey: From Diagnosis to Awareness
The Diagnosis
Coulier disclosed that he had been feeling fatigued and unwell for several months before seeking medical advice.
A series of diagnostic tests, including a biopsy and imaging scans, confirmed the presence of Stage 3 Non-Hodgkin’s Lymphoma.
How He Shared the News
In a heartfelt video shared with his fans, Coulier discussed his diagnosis candidly. The star emphasized the importance of listening to one’s body and seeking medical help when something feels off.
“I’ve always tried to make people laugh, but now, I want to use my voice to educate and inspire,” he said.
Symptoms of Non-Hodgkin’s Lymphoma
Recognizing the symptoms early can make a significant difference in treatment outcomes.
Some common symptoms include:
- Swollen lymph nodes, often painless
- Persistent fatigue
- Unexplained weight loss
- Fever and night sweats
- Abdominal pain or swelling
- Chest pain, coughing, or trouble breathing
Why Early Detection Matters
Coulier’s journey highlights the importance of not ignoring persistent symptoms. Timely diagnosis can improve treatment effectiveness and overall prognosis.
Stages of Non-Hodgkin’s Lymphoma
NHL is categorized into four stages based on its spread:
- Stage 1: Cancer is localized to one lymph node region.
- Stage 2: Two or more lymph node regions on the same side of the diaphragm are affected.
- Stage 3: Cancer involves lymph nodes on both sides of the diaphragm.
- Stage 4: The disease has spread beyond the lymphatic system to other organs.
Coulier’s diagnosis at Stage 3 underscores the critical need for awareness and early intervention.
Treatment Options for Non-Hodgkin’s Lymphoma
Tailored Treatment Plans
The treatment for NHL varies depending on the stage and specific subtype.
Common approaches include:
- Chemotherapy: Often the first line of defense to target rapidly dividing cancer cells.
- Radiation Therapy: Used to shrink tumors in localized areas.
- Immunotherapy: Boosts the immune system’s ability to fight cancer.
- Targeted Therapy: Focuses on specific molecules involved in cancer growth.
Dave Coulier’s Treatment Regimen
While Coulier hasn’t shared detailed specifics about his treatment, he expressed gratitude for his medical team and the support of loved ones.
Living with Non-Hodgkin’s Lymphoma
Physical and Emotional Challenges
Coping with cancer involves more than just physical treatments. Patients often face emotional struggles, including anxiety, fear, and uncertainty.
Coulier’s Positive Outlook
Despite his diagnosis, Coulier remains optimistic, often sharing moments of humor and gratitude. His resilience inspires others battling similar challenges.
Raising Awareness for Non-Hodgkin’s Lymphoma
The Power of Advocacy
Coulier is using his platform to spread awareness about NHL. His message encourages individuals to prioritize their health and support ongoing cancer research.
Supporting Research and Treatment Advances
Progress in lymphoma treatment, such as CAR T-cell therapy and advancements in immunotherapy, offers hope for patients worldwide.
How Fans Can Show Their Support
Messages of Encouragement
Fans have flooded social media with messages of love and encouragement for Coulier. Sharing personal stories of resilience and hope strengthens the community of those affected by lymphoma.
Donating to Lymphoma Research
Supporting organizations focused on lymphoma research and patient advocacy can make a significant impact.
Conclusion:
Dave Coulier’s openness about his battle with Stage 3 Non-Hodgkin’s Lymphoma reminds us of the importance of health awareness and community support. As he navigates this challenging chapter, his strength and advocacy serve as a beacon of hope for others facing similar battles.
FAQs
1. Can Non-Hodgkin’s Lymphoma be cured?
Yes, many cases of NHL can be treated effectively, especially when diagnosed early. Advanced treatments have improved survival rates significantly.
2. How does Non-Hodgkin’s Lymphoma differ from Hodgkin’s Lymphoma?
The primary difference lies in the specific type of cancerous cells. Hodgkin’s Lymphoma involves Reed-Sternberg cells, which are absent in NHL.
3. Are there lifestyle factors that increase the risk of NHL?
While the exact cause is unknown, factors like a weakened immune system, certain infections, and exposure to specific chemicals can increase risk.
4. What support resources are available for NHL patients?
Numerous organizations, such as the Lymphoma Research Foundation, offer resources, support groups, and financial assistance for patients and their families.
5. How can I reduce my risk of developing lymphoma?
Maintaining a healthy lifestyle, avoiding exposure to harmful chemicals, and addressing infections promptly can help lower your risk.
References:
-

 Trending Stories1 year ago
Trending Stories1 year agoCDC: 1 in 4 Americans Still COVID-Free by End of 2022
-

 Health8 months ago
Health8 months agoHow Do Pawpaw Seeds Support Cardiovascular Health?
-

 Health5 years ago
Health5 years agoMeghan Trainor Shares Motivational New Song ‘Blink’
-

 Health2 years ago
Health2 years agoHow Long Does Monkey Pox Last Before It Surfaces in the Body?
-

 Health3 years ago
Health3 years agoWhat Causes Swollen Body? Understanding Edema and its Triggers
-

 Health3 years ago
Health3 years agoNutrition and the Importance of a Fitness Program – 3 Things to Know
-

 Health3 years ago
Health3 years ago5 Weird Reasons Why Pimples Disappear After Marriage
-

 Health3 years ago
Health3 years agoHealth Benefits Of Pawpaw Seed? 7 Things To Know






