Health
How diabetes retinopathy prevention can help you prevent blindness

How diabetes retinopathy prevention can help you prevent blindness
As you know, diabetes can lead to a range of complications, one of which is vision loss. If left untreated, diabetic retinopathy can progress and cause vision loss in different ways.
In this post, we’ll focus on the different types of vision loss that can be caused by diabetes, as well as the various ways in which you can prevent them.
We’ll also provide you with specific tips and advice on how to detect and treat diabetic retinopathy. So if your vision is important to you, be sure to read on!
What causes diabetes blindness?

If you’re diabetic, you know all too well the risk of developing diabetes blindness. Diabetes damages the blood vessels in the eye, which can lead to vision loss.
There are many ways to prevent diabetes blindness, including taking medication and following a healthy lifestyle. If your eyesight starts to deteriorate, don’t wait – get treatment right away!
Always talk to your physician about your risk for developing diabetes blindness and how best to prevent it.
Keep in mind that there’s no one-size-fits-all approach to preventing diabetes blindness, so be proactive and research the best ways to protect your vision and health.
How diabetes retinopathy prevention can help you prevent blindness

Diabetes retinopathy Prevention is a program that can help you prevent blindness from developing in people with diabetes.
The program includes screenings and early detection of diabetic eye disease, treatment if needed, and follow-up care to ensure prevention success.
By participating in the program, you can save your vision and avoid becoming blind later on in life.
Getting involved today is the best way to start your journey to preventing blindness – book an appointment at your local health center or call 1-800-222-1222 for more information.
The kinds of treatments for diabetes retinopathy

Preventing blindness from diabetic retinopathy is possible with the right treatment. There are many types of treatments available, and each has its own benefits.
Some common treatments include laser surgery, photodynamic therapy (PDT), and cryotherapy. Each treatment is effective in different ways and can be tailored to the individual patient’s needs.
By choosing the right treatment option, you can help prevent blindness from turning into a lifelong disability.
Keep in mind that treatment options vary depending on the severity of diabetic retinopathy and the level of vision loss.
So, it’s important to consult with your doctor to determine the best course of action for you.
Three types of diabetes retinopathy
Diabetes retinopathy is a condition that can lead to blindness if not treated promptly. It is important to know the symptoms of diabetic retinopathy so that you can take action and prevent the condition from developing.
There are three types of diabetes retinopathy – nephropathy, neuropathy, and ophthalmia. Nephropathy is the most common type, and it is caused by blood sugar levels becoming too high.
Neuropathy is a condition in which the nerves are damaged, and ophthalmia is the most severe type, which can lead to blindness.
It’s important to keep blood sugar levels under control and monitor your blood pressure and blood sugar levels regularly.
If you experience any of the following symptoms, it’s important to see your doctor immediately: changes in your vision, eye pain, redness of the eye, eye swelling, or discharge from the eye.
Prevention is key to keeping your vision healthy and preventing blindness in future generations!
Diabetes retinopathy prevention tips

Preventing blindness due to diabetic retinopathy is possible with good eye care. Follow these tips to keep your vision healthy:
- Keep your eyes healthy by following the eye care guidelines outlined in the American Diabetes Association (ADA) publication, “Eating Well With diabetes.”
- Get regularly checked for early signs of diabetic retinopathy (DR). If you notice any changes in your vision, get treatment right away.
- Limit your sugar and carbohydrate intake to stop the growth of diabetic retinopathy cells.
- Take regular breaks from the computer screen and other bright lights to reduce eye fatigue.
- What other problems can diabetic retinopathy cause?
Preventing diabetic retinopathy is essential if you want to keep your vision healthy. This eye disease can cause problems with your vision, such as night blindness and blurry vision.
In some cases, diabetic retinopathy may even lead to the need for a blind person to have surgery. However, by taking good care of yourself and your blood sugar levels, you can reduce your risk of developing diabetic retinopathy in the first place.
Here are some other ways that you can help prevent diabetic retinopathy:
Am I at risk for diabetic retinopathy?

If you have diabetes, it’s important to know your risk factors for diabetic retinopathy. This eye disease can lead to blindness, and it’s on the rise among people with diabetes.
Prevention is the key to preventing this devastating condition, so it’s crucial to know what you’re at risk for.
If you have diabetes and are at high risk for developing diabetic retinopathy, there are a few things you can do to reduce your chances.
For example, make sure to get regular eye exams and treatment if you detect signs of the disease early on.
And last but not least, make sure to listen to your doctor and take all of his or her recommendations seriously.
By doing these simple things, you can help prevent blindness and safeguard your vision for years to come.
How will my eye doctor check for diabetic retinopathy?
Preventing diabetes-related blindness starts with good eye health. That’s why it’s important to have regular screenings for blood vessel conditions like diabetic retinopathy.
If you’re at high risk, your doctor may also recommend treatment such as laser eye surgery or eye drops. In some cases, early diagnosis and treatment can prevent the progression of the disease.
However, no matter how well you take care of your eyes, the risk of blindness remains high for people with diabetes.
That’s why it’s important to be proactive and make lifestyle changes, such as eating a balanced diet and exercising regularly, to help reduce your chances of developing the disease in the first place.
What can I do to prevent diabetic retinopathy?
There is no one-size-fits-all answer when it comes to preventing diabetic retinopathy, as the best way to prevent this condition depends on the individual.
However, there are a few things that everyone with diabetes should do to increase their chances of avoiding vision problems down the line.
Firstly, make sure to get regular eye exams and treat any vision problems early. Secondly, maintain a healthy weight and eat a balanced diet that includes plenty of fruits and vegetables.
Thirdly, if you have diabetes, be sure to keep your blood glucose levels under control with insulin therapy and exercise regularly.
And lastly, preventive care is the key to preventing blindness in people with diabetes mellitus – by regularly monitoring your blood sugar levels and getting regular eye exams, you can help keep your vision healthy and functional.
What’s the treatment for diabetic retinopathy and DME?

Preventing blindness from diabetic retinopathy is crucial, and there are many different treatment options available.
Depending on the severity of the condition, you may need multiple treatment sessions over time to achieve optimal results.
Make sure you take the time to learn about the different treatment options and make the best decision for your individual situation.
Prevention is key – make sure you take steps to avoid developing this condition in the first place!
What is the latest research on diabetic retinopathy and DME?

Preventing blindness is one of the key priorities for people with diabetes. And one of the most effective ways to do it is by preventing diabetic retinopathy.
Diabetic retinopathy is a leading cause of blindness in people with diabetes, and the incidence is on the rise. Fortunately, there are many ways to prevent it – including taking proper care of your eyesight and eating a healthy diet.
The latest research shows that DME (diabetic Mellitus exercise) can be very effective in preventing eye disease in people with diabetes.
This type of exercise not only helps improve blood sugar control but also reduces the risk of vascular complications such as stroke and heart attack.
So, if you are looking to protect your vision and prevent blindness, make sure to include DME in your daily routine!
Diabetic Eye Disease Resources

Preventing blindness from occurring as a result of diabetic retinopathy is possible with the help of proper eye care and lifestyle choices.
diabetic retinopathy prevention resources can help you on your way to a healthier and longer life. One of the most common problems associated with diabetes is eye disease, which can lead to blindness.
If you’re at risk, make sure to get regular screenings for diabetic retinopathy and take action if necessary.
By knowing the warning signs, you can live a healthier life and prevent blindness from happening in the future!
Who is at risk of diabetic retinopathy?

If you have diabetes, you’re at risk for diabetic retinopathy. Diabetic retinopathy is a condition that affects the blood vessels in your eyes, and if left untreated can lead to blindness.
Although it’s more common in people with diabetes, diabetic retinopathy can affect anyone. Left untreated, diabetic retinopathy can cause eye blood vessels to thicken and leak, which can cause vision problems.
Fortunately, there are ways to prevent and treat diabetic retinopathy so you don’t have to worry about losing your vision.
Make sure to get regular eye exams and treatment for diabetic retinopathy as soon as you notice any changes, and don’t hesitate to talk to your doctor if you have any questions.
How is diabetic retinopathy treated?

Diabetic retinopathy is a complication of diabetes that can lead to blindness. If you’re diabetic and have high blood sugar levels, you’re at risk of developing the condition.
Diabetic retinopathy is the most common vision problem in people with diabetes. It’s a build-up of fluid and blood in the eye, which can cause vision loss and blindness.
There are several ways to prevent diabetic retinopathy, including taking care of your blood sugar levels and eye health.
Treatment typically includes laser treatment and surgery to remove the thickened retinae. Keeping your eyes healthy throughout your lifetime is the best way to avoid developing diabetic retinopathy in the first place!
So make sure to get regular eye exams and follow all the doctor’s instructions to stay on the right track.
Get a diabetic eye exam once a year

It is important to get a diabetic eye exam once a year to monitor your progress and catch early signs of diabetic retinopathy. If you are at risk for this complication, make sure to get checked every three months.
Prevention of the development of diabetic retinopathy mainly relies on taking good care of your eyes by following regular diet and exercise guidelines as well as using medication when needed.
However, no matter how diligent you are, there’s always the chance that something will go wrong eventually. So it is essential to have regular eye exams in case any problems do arise.
Doing so can help save your vision from deteriorating completely
Follow your diabetes management plan

Treating diabetic retinopathy involves a combination of laser therapy, surgery, and medications. If you are not following your diabetes management plan, you might not be getting the best possible care and could be risking your vision.
Make sure to visit your doctor regularly for check-ups and updates on your treatment progress – this way, you will know whether or not the treatments are having the desired effect.
PDR (proliferative diabetic retinopathy)
PDR is a complication that results from high blood sugar levels. It can lead to blindness if left untreated. There are various treatments available, depending on the stage of PDR.
You need to consult with an expert and start treatment as soon as possible in order to prevent vision loss.
What Happens When You Have Diabetic Retinopathy?

Preventing blindness is a top priority for anyone with diabetes, and diabetic retinopathy is the leading cause of blindness in adults over the age of 50.
If left untreated, diabetic retinopathy can progress to macular edema, retinal detachment, and even loss of vision. Here are four key things you can do to help protect your vision and prevent diabetic retinopathy from becoming a reality:
Can Diabetic Retinopathy Go Away?

There is no question that diabetes retinopathy prevention can help you prevent blindness. Diabetes retinopathy is a disease that affects the retina and can lead to vision loss.
There are many ways to prevent it, including following proper eye care, diet, and exercise. However, if you notice any changes in your vision or if diabetes retinopathy prevention isn’t working anymore, it is important to seek professional medical help.
Diabetic retinopathy is a serious condition and needs to be treated as soon as possible to prevent permanent vision loss.
5 Ways to Prevent Vision Loss from Diabetic Retinopathy
Preventing vision loss from diabetic retinopathy is important for everyone, but is especially vital for those with the disease. Here are five ways to help you prevent vision loss from diabetic retinopathy:
Do You Have Diabetes and Need an Eyeglasses Exam?

Preventing diabetes retinopathy is important because it can reduce the likelihood of developing blindness as a result of your diabetes. If you do develop diabetic retinopathy, there are several ways you can prevent or treat it.
Some of the most common methods include using oral medications, wearing glasses, and undergoing laser therapy. If you’re at risk for developing diabetic retinopathy, it’s important to know about the risks and take steps to prevent blindness from happening.
For example, have an annual eye exam to check for signs of diabetic retinopathy and get treatment if necessary. Remember, prevention is the best way to avoid problems!
Preventing diabetic retinopathy
 Preventing diabetic retinopathy is key if you have diabetes. This condition, which is the leading cause of blindness in adults over 50 years old, is typically caused by high blood sugar levels and can be prevented by following a healthy diet and regular eye exams and checkups.
Preventing diabetic retinopathy is key if you have diabetes. This condition, which is the leading cause of blindness in adults over 50 years old, is typically caused by high blood sugar levels and can be prevented by following a healthy diet and regular eye exams and checkups.
If you do develop diabetic retinopathy, make sure to get treatment as soon as possible to prevent vision loss. By taking these simple steps, you can help protect your eyesight and live a longer life!
Frequently Asked Questions
What are the signs and symptoms of diabetic retinopathy?
If you have diabetes and develop diabetic retinopathy, the symptoms can include blurred vision, red eyes, and night blindness.
If you notice any of these symptoms, it’s important to see a doctor as soon as possible. Treatment for the condition usually requires laser surgery or ophthalmic injections.
What can I do to reduce my risk of developing diabetes retinopathy?
If you are a type 1 diabetic and you are experiencing poor blood sugar control, then make sure to monitor your blood sugar levels and follow the dietary advice given by your doctor. In addition, if you need glasses or contact lenses for distance vision, make sure that you wear them.
You can also reduce your risk of developing diabetic retinopathy by getting enough exercise. Even just 30 minutes of activity every day is recommended.
Additionally, get regular checkups and treatment for this eye condition as early as possible to avoid complications down the line.
How can I treat or prevent diabetic retinopathy with surgery?
If you have type 2 diabetes and are at high risk for developing diabetic retinopathy, it is important to get screened for the condition. If you are diagnosed with the disease, laser surgery can be performed to reduce or stop its progression.
Additional treatments like PDT (photodynamic therapy) and PRK (photorefractive keratectomy) may also be recommended in order to halt or improve vision.
Can oral medications help me prevent diabetic retinopathy?
Yes, oral medications like metformin and tetracycline can help prevent diabetic retinopathy. Both of these medications work by altering blood sugar levels in diabetes patients.
Metformin works by decreasing blood sugar levels, while tetracycline tightens blood vessels which reduces the level of blood sugar in the blood.
By taking these medications regularly, you’ll significantly lower your chances of developing diabetic retinopathy over time.
In addition, these medications can also improve vision as blood sugar levels are controlled in a healthy way.
Are there any other measures that I should take to prevent diabetic retinopathy?
There are a few measures you can take to prevent diabetic retinopathy. Make sure to eat a healthy diet and get enough exercise.
Additionally, make sure to avoid smoking, drinking alcohol excessively, and using illegal drugs.
When it comes to diabetes retinopathy prevention, you should also wear sunglasses when outdoors in direct sunlight for long periods of time.
Get screened for diabetes every year by your doctor and have an annual eye exam.
Conclusion
Diabetes retinopathy is a condition that can lead to vision loss, and it is important to take preventative measures to avoid this.
By understanding the different types of diabetic retinopathy and the various treatments available, you can ensure that you remain sighted throughout your life.
If you are concerned about your vision or have diabetes, make an appointment with your doctor for an eye exam. In the meantime, scroll down for some helpful diabetes retinopathy prevention tips.
Health
Understanding the Risk Factors for Developing Preeclampsia
Understanding the Risk Factors for Developing Preeclampsia
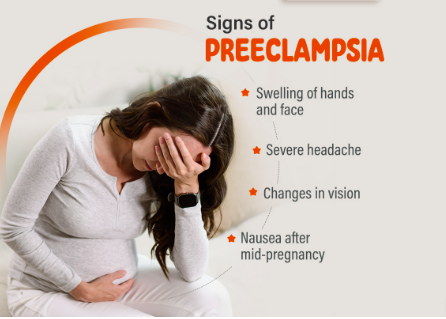
Preeclampsia is a serious pregnancy complication characterized by high blood pressure and potential damage to organs such as the liver and kidneys.
It usually occurs after the 20th week of pregnancy and can have significant implications for both the mother and the baby.
Identifying the risk factors associated with preeclampsia is crucial for early intervention and management.
This article delves into the various risk factors, how they contribute to the development of preeclampsia and strategies for monitoring and prevention.
What Is Preeclampsia?
Preeclampsia is a condition that affects approximately 5-8% of pregnancies worldwide. It typically manifests with elevated blood pressure and proteinuria (excess protein in the urine).
If left untreated, it can lead to severe complications such as eclampsia, which involves seizures and can jeopardize both maternal and fetal health.
Risk Factors for Preeclampsia
Understanding the risk factors for preeclampsia can help in early diagnosis and management. Below are the primary risk factors associated with this condition:
1. Previous History of Preeclampsia
Women who have experienced preeclampsia in previous pregnancies are at a higher risk of developing the condition in subsequent pregnancies. The recurrence risk is approximately 20-30% if preeclampsia occurs in a previous pregnancy.
2. First Pregnancy
The risk of preeclampsia is higher in women who are pregnant for the first time. This is thought to be related to the body’s adjustment to the physiological changes associated with pregnancy.
3. Advanced Maternal Age
Women who are over the age of 35 are more likely to develop preeclampsia. The increased risk is associated with age-related changes in blood vessels and the body’s ability to manage pregnancy-related stress.
4. Multiple Gestations
Carrying more than one baby (e.g., twins or triplets) increases the risk of preeclampsia. The body’s increased demands and altered placental development contribute to this heightened risk.
5. Obesity
Obesity is a significant risk factor for preeclampsia. Excess body weight can lead to increased blood pressure and insulin resistance, both of which are associated with a higher likelihood of developing preeclampsia.
6. Chronic Hypertension
Women with pre-existing high blood pressure are at a greater risk of developing preeclampsia. Chronic hypertension can exacerbate the blood pressure problems associated with preeclampsia.
7. Diabetes
Both type 1 and type 2 diabetes are associated with an increased risk of preeclampsia. Diabetes can affect blood vessel function and increase the likelihood of high blood pressure during pregnancy.
8. Kidney Disease
Pre-existing kidney conditions can elevate the risk of preeclampsia. The kidneys play a crucial role in managing blood pressure and fluid balance, and any pre-existing conditions can compromise their function.
9. Autoimmune Disorders
Certain autoimmune disorders, such as lupus and rheumatoid arthritis, can increase the risk of developing preeclampsia. These conditions can affect the body’s immune response and vascular health.
10. Family History
A family history of preeclampsia can indicate a genetic predisposition to the condition. Women with a family history are at an increased risk compared to those without such a history.
11. Poor Nutrition
Inadequate nutrition, particularly a lack of essential vitamins and minerals such as calcium and magnesium, can contribute to the development of preeclampsia. Proper prenatal care and nutrition are crucial for minimizing risk.
12. Infections
Certain infections during pregnancy, such as urinary tract infections, can be associated with an increased risk of preeclampsia. Infections can exacerbate the inflammatory processes involved in preeclampsia.
13. High Stress Levels
Chronic stress and poor mental health can impact overall well-being and contribute to conditions like preeclampsia. Managing stress through healthy lifestyle choices and support systems is important.
Monitoring and Prevention Strategies
Early monitoring and preventive measures can help manage the risk factors associated with preeclampsia:
- Regular Prenatal Visits: Frequent check-ups with a healthcare provider can help monitor blood pressure and other indicators of preeclampsia.
- Healthy Lifestyle Choices: Maintaining a balanced diet, engaging in regular physical activity, and managing weight can reduce the risk.
- Medication: In some cases, medications such as aspirin may be recommended to lower the risk of preeclampsia, especially for women with a high risk.
- Stress Management: Techniques such as mindfulness, relaxation exercises, and counseling can help manage stress and support overall health.
- Education and Awareness: Understanding the symptoms and risk factors of preeclampsia can help in early detection and timely intervention.
Conclusion
Preeclampsia is a complex condition with multiple risk factors. By recognizing these factors and taking proactive steps, expectant mothers can work with their healthcare providers to manage their risk and promote a healthier pregnancy.
Regular prenatal care, lifestyle modifications, and stress management are key to minimizing the impact of preeclampsia and ensuring the best possible outcomes for both mother and baby.
FAQs
1. What are the early signs of preeclampsia?
Early signs of preeclampsia include high blood pressure, proteinuria, swelling of the hands and feet, sudden weight gain, and severe headaches. It’s important to report any unusual symptoms to your healthcare provider promptly.
2. Can preeclampsia be prevented?
While not all cases of preeclampsia can be prevented, maintaining a healthy lifestyle, attending regular prenatal visits, and following your healthcare provider’s recommendations can help reduce the risk.
3. How is preeclampsia diagnosed?
Preeclampsia is diagnosed through routine prenatal screenings that monitor blood pressure and urine protein levels. If preeclampsia is suspected, additional tests may be conducted to assess kidney function and other health indicators.
4. What are the treatment options for preeclampsia?
Treatment options for preeclampsia depend on the severity of the condition. They may include medications to manage blood pressure, bed rest, and in severe cases, early delivery of the baby to protect both the mother and child.
5. Can preeclampsia affect future pregnancies?
Having preeclampsia in one pregnancy can increase the risk of developing it in future pregnancies. However, many women go on to have healthy pregnancies by managing risk factors and following their healthcare provider’s advice.
References:
Health
Top 5 Immunity-Boosting Fruits to Include in Your Diet

Top 5 Immunity-Boosting Fruits to Include in Your Diet
In our quest for better health, the immune system often takes center stage. One of the simplest and most effective ways to support this vital system is through a nutritious diet.
Fruits, rich in essential vitamins, minerals, and antioxidants, can play a significant role in strengthening your immune system.
In this article, we’ll explore the best fruits for boosting immunity, backed by scientific research, and provide practical tips for incorporating them into your daily routine.
Why Immune Health Matters
The immune system is our body’s defense mechanism against harmful pathogens, including bacteria, viruses, and toxins.
A robust immune system can help fend off illnesses and infections, and a balanced diet is crucial for maintaining its optimal function.
Fruits, in particular, offer a wealth of nutrients that can enhance immune response, improve overall health, and even prevent chronic diseases.
1. Citrus Fruits: Vitamin C Powerhouses
Oranges
Oranges are synonymous with vitamin C, a crucial nutrient for immune health. Vitamin C supports the production and function of white blood cells, which are essential for fighting infections.
Just one medium-sized orange provides about 70 mg of vitamin C, meeting the daily recommended intake for most adults.
Grapefruits
Grapefruits, another excellent source of vitamin C, also contain antioxidants like lycopene, which have been linked to reduced inflammation and improved immune function.
Enjoying half a grapefruit a day can contribute significantly to your vitamin C needs.
Lemons
Lemons are versatile fruits that not only boost your vitamin C intake but also support detoxification.
Adding lemon juice to water or dishes can enhance your immune system while providing a refreshing flavor.
2. Berries: Antioxidant-Rich Superfoods
Blueberries
Blueberries are packed with antioxidants, particularly flavonoids, which help combat oxidative stress and inflammation.
These antioxidants can enhance immune function and protect against chronic diseases. A cup of fresh blueberries is a delicious way to boost your immunity.
Strawberries
Strawberries are another berry with a high vitamin C content, along with various antioxidants that contribute to overall health.
A handful of strawberries can provide a significant portion of your daily vitamin C requirement.
Raspberries
Raspberries are rich in vitamins C and E, as well as fiber and antioxidants.
These nutrients work together to support immune health and maintain digestive well-being.
Incorporate raspberries into smoothies or salads for a tasty immune boost.
4. Papaya
Papaya is an excellent source of vitamin C, vitamin A, and digestive enzymes such as papain. These nutrients contribute to a stronger immune system by supporting cellular repair and reducing inflammation.
5. Pomegranate
Pomegranates are rich in antioxidants and vitamin C, which help combat oxidative stress and boost immune function. The anti-inflammatory properties of pomegranates also support overall health and wellness.
Incorporating these fruits into your daily diet can provide essential nutrients that support immune health and help protect your body against illnesses.
Frequently Asked Questions
1. How does vitamin C boost the immune system?
Vitamin C enhances the production of white blood cells, which are crucial for combating infections and illnesses. It also acts as an antioxidant, protecting cells from damage caused by free radicals.
2. Can berries help reduce inflammation?
Yes, berries are rich in antioxidants and vitamins that help reduce inflammation and oxidative stress, which can support overall immune function.
3. What are the benefits of kiwi for immune health?
Kiwi provide a high amount of vitamin C, which supports the immune system by increasing white blood cell production. It also contains vitamin K and folate, which are essential for maintaining overall health.
4. How does papaya contribute to immune health?
Papaya is high in vitamin C and vitamin A, which help strengthen the immune system. Additionally, the enzyme papain in papaya aids in digestion and reduces inflammation.
5. What makes pomegranates beneficial for immunity?
Pomegranates are rich in antioxidants and vitamin C, which help fight oxidative stress and inflammation, thereby supporting the immune system and overall health.
References:
Healthline – Best Fruits for Boosting Immunity
Health
Effective Medications to Lower Cholesterol: A Comprehensive Guide

Effective Medications to Lower Cholesterol: A Comprehensive Guide
High cholesterol is a common health issue that can significantly increase the risk of heart disease, stroke, and other serious health conditions. Fortunately, various medications are available to help manage and lower cholesterol levels.
In this guide, we’ll explore the most effective medications for lowering cholesterol, their mechanisms of action, potential side effects, and other crucial information to help you make informed decisions about your health.
Understanding Cholesterol and Its Impact on Health
Cholesterol is a fatty substance found in your blood. Your body needs cholesterol to build healthy cells, but having high levels of cholesterol can increase your risk of heart disease.
Cholesterol travels through your bloodstream in two main types of lipoproteins:
low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
- LDL Cholesterol: Often referred to as “bad” cholesterol, LDL can build up in the walls of your arteries, leading to atherosclerosis, which can restrict blood flow and increase the risk of heart attacks and strokes.
- HDL Cholesterol: Known as “good” cholesterol, HDL helps remove LDL cholesterol from your arteries, reducing the risk of cardiovascular problems.
Why Medication May Be Necessary
Even with a healthy diet and regular exercise, some individuals may still struggle to manage their cholesterol levels.
This is where cholesterol-lowering medications come into play. These medications work in various ways to help lower LDL cholesterol and, in some cases, raise HDL cholesterol.
Types of Cholesterol-Lowering Medications
1. Statins
Statins are the most commonly prescribed medications for lowering LDL cholesterol.
They work by blocking a substance your body needs to make cholesterol, thus reducing the amount of LDL cholesterol in your bloodstream.
- Examples: Atorvastatin (Lipitor), Simvastatin (Zocor), Rosuvastatin (Crestor)
- Mechanism of Action: Statins inhibit the enzyme HMG-CoA reductase, which is involved in cholesterol production in the liver.
- Common Side Effects: Muscle pain, digestive problems, increased liver enzymes
- Benefits: Statins are highly effective in reducing LDL cholesterol levels and have been shown to lower the risk of heart attacks and strokes.
2. Bile Acid Sequestrants
Bile acid sequestrants work by binding to bile acids in the intestine, preventing them from being reabsorbed. This process forces the liver to use cholesterol to produce more bile acids, thus lowering LDL cholesterol levels.
- Examples: Cholestyramine (Prevalite), Colestipol (Colestid), Colesevelam (Welchol)
- Mechanism of Action: These drugs bind bile acids in the intestines, reducing cholesterol absorption.
- Common Side Effects: Constipation, bloating, nausea
- Benefits: Effective at lowering LDL cholesterol and can be used in conjunction with statins for enhanced results.
3. Niacin
Niacin (also known as vitamin B3) helps lower LDL cholesterol and raise HDL cholesterol levels.
It works by decreasing the liver’s production of LDL cholesterol and increasing HDL cholesterol.
- Examples: Niacor, Niaspan
- Mechanism of Action: Niacin reduces the production of LDL cholesterol and increases HDL cholesterol.
- Common Side Effects: Flushing, itching, liver damage (with high doses)
- Benefits: Effective in raising HDL cholesterol and lowering LDL cholesterol.
4. Fibric Acids
Fabric acids, or fibrates, are primarily used to lower triglyceride levels and can also help increase HDL cholesterol levels.
They work by activating a protein that helps break down triglycerides in the blood.
- Examples: Fenofibrate (Tricor), Gemfibrozil (Lopid)
- Mechanism of Action: They activate peroxisome proliferator-activated receptors (PPARs), which help in the breakdown of triglycerides.
- Common Side Effects: Muscle pain, liver abnormalities, gastrointestinal issues
- Benefits: Particularly useful for individuals with high triglyceride levels.
5. PCSK9 Inhibitors
PCSK9 inhibitors are a newer class of cholesterol-lowering medications that help the liver remove LDL cholesterol from the bloodstream more effectively.
- Examples: Alirocumab (Praluent), Evolocumab (Repatha)
- Mechanism of Action: These drugs inhibit the PCSK9 protein, which normally reduces the liver’s ability to remove LDL cholesterol from the blood.
- Common Side Effects: Injection site reactions, flu-like symptoms
- Benefits: Very effective at lowering LDL cholesterol, especially in individuals who cannot tolerate statins.
6. Cholesterol Absorption Inhibitors
Cholesterol absorption inhibitors work by blocking the absorption of cholesterol from the diet, which reduces the amount of cholesterol that enters your bloodstream.
- Examples: Ezetimibe (Zetia)
- Mechanism of Action: They inhibit the absorption of cholesterol in the small intestine.
- Common Side Effects: Diarrhea, stomach pain, muscle pain
- Benefits: Can be used alone or in combination with statins to lower LDL cholesterol.
Choosing the Right Medication
The choice of medication depends on various factors, including your overall health, the specific cholesterol issue you have, and how well you tolerate certain medications.
Your healthcare provider will help you determine the most appropriate medication based on your individual needs and medical history.
Lifestyle Modifications to Complement Medication
While medications are effective in managing cholesterol levels, they work best when combined with lifestyle changes.
Consider incorporating the following into your routine:
- Healthy Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins while avoiding saturated fats and trans fats.
- Regular Exercise: Engage in at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week.
- Weight Management: Achieve and maintain a healthy weight to help control cholesterol levels.
- Avoid Smoking and Limit Alcohol: Both smoking and excessive alcohol intake can negatively impact cholesterol levels.
Monitoring and Follow-Up
Regular follow-up with your healthcare provider is crucial to monitor your cholesterol levels and assess the effectiveness of your medication. Your doctor may adjust your treatment plan based on your progress and any side effects you experience.
Final Thoughts
Managing cholesterol is a critical aspect of maintaining cardiovascular health.
With a variety of effective medications available, it’s possible to lower LDL cholesterol levels and reduce the risk of heart disease and other complications.
However, medication alone is not a cure-all; combining it with lifestyle changes is essential for optimal results.
Always consult your healthcare provider for personalized advice and treatment plans tailored to your specific needs.
Frequently Asked Questions (FAQs)
1. What is the primary goal of cholesterol-lowering medications?
Cholesterol-lowering medications primarily aim to reduce LDL cholesterol levels in the blood, thereby decreasing the risk of cardiovascular diseases such as heart attacks and strokes.
2. Are there any natural alternatives to cholesterol-lowering medications?
Yes, some natural alternatives include dietary changes (e.g., increased intake of soluble fiber and omega-3 fatty acids), regular exercise, and weight management. However, these should be used in conjunction with, not as a replacement for, prescribed medications.
3. How long does it take for cholesterol-lowering medications to show results?
The effects of cholesterol-lowering medications can usually be observed within a few weeks, but it may take several months to see significant changes in cholesterol levels and overall cardiovascular risk.
4. Can cholesterol-lowering medications cause side effects?
Yes, some common side effects include muscle pain, digestive issues, and liver enzyme changes. It’s important to report any side effects to your healthcare provider for proper management.
5. Can I stop taking my cholesterol medication if my levels improve?
It’s important to consult your healthcare provider before making any changes to your medication regimen. Discontinuing medication without medical advice can lead to a rebound in cholesterol levels and an increased risk of heart disease.
References
Cholesterol-lowering Medications
-

 Trending Stories1 year ago
Trending Stories1 year agoCDC: 1 in 4 Americans Still COVID-Free by End of 2022
-

 Health5 years ago
Health5 years agoMeghan Trainor Shares Motivational New Song ‘Blink’
-

 Health2 years ago
Health2 years agoHow Long Does Monkey Pox Last Before It Surfaces in the Body?
-

 Health2 years ago
Health2 years agoWhat Causes Swollen Body? Understanding Edema and its Triggers
-

 Health3 years ago
Health3 years agoNutrition and the Importance of a Fitness Program – 3 Things to Know
-

 Health3 years ago
Health3 years ago5 Weird Reasons Why Pimples Disappear After Marriage
-

 Health3 months ago
Health3 months agoHow Do Pawpaw Seeds Support Cardiovascular Health?
-

 Health2 years ago
Health2 years agoHealth Benefits Of Pawpaw Seed? 7 Things To Know





