Health
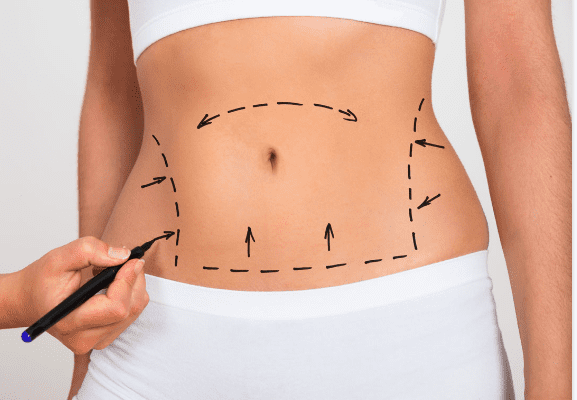
What Weight Loss Surgery is Best For the Body?
Last Updated on May 16, 2023 by Nurse Vicky
What Weight Loss Surgery is Best For the Body?
In today’s fast-paced world, weight loss has become a significant concern for many individuals. While various methods exist to shed excess pounds, weight loss surgery has gained prominence as an effective solution for individuals struggling with obesity.
This article aims to unravel the mystery surrounding weight loss surgeries and provide detailed information on the different types of surgeries available, their benefits, risks, and considerations to help you make an informed decision.
Understanding Weight Loss Surgeries and Their Purpose
Weight loss surgeries, also known as bariatric surgeries, are medical procedures designed to help individuals achieve significant and sustained weight loss by altering the digestive system.
These surgeries work by restricting the amount of food the stomach can hold or by limiting the absorption of nutrients. The primary purpose of weight loss surgeries is to improve overall health and reduce the risk of obesity-related health conditions, such as diabetes, high blood pressure, and heart disease. Different Types of Weight Loss Surgeries
Gastric Bypass Surgery
Gastric bypass surgery is one of the most common and effective weight loss procedures. During this surgery, the surgeon creates a small pouch at the top of the stomach and connex cts it directly to the middle portion of the small intestine, bypassing a significant portion of the stomach and upper small intestine. This results in reduced food intake and decreased nutrient absorption.
Sleeve Gastrectomy
Sleeve gastrectomy involves removing a large portion of the stomach, leaving behind a smaller sleeve-shaped stomach. This procedure restricts food intake by reducing the stomach’s size and removing the part responsible for producing hunger-inducing hormones.
Adjustable Gastric Banding
Adjustable gastric banding is a reversible weight loss surgery that involves placing an inflatable band around the upper part of the stomach, creating a small pouch. The band can be adjusted to control food intake by tightening or loosening it. This procedure does not involve any removal of stomach tissue.
Biliopancreatic Diversion with Duodenal Switch
This complex weight loss surgery involves removing a significant portion of the stomach and rerouting the small intestine to limit both food intake and nutrient absorption. It is usually recommended for individuals with a high body mass index (BMI). Factors to Consider Before Undergoing Weight Loss Surgery
Eligibility and Evaluation
Before undergoing weight loss surgery, individuals are evaluated by healthcare professionals to determine their eligibility. Factors such as BMI, medical history, previous weight loss attempts, and overall health are taken into account. It’s important to consult with a qualified surgeon to assess your suitability for surgery.
Potential Risks and Complications
Like any surgical procedure, weight loss surgeries carry risks. These may include infection, bleeding, blood clots, and adverse reactions to anesthesia. Additionally, long-term complications such as malnutrition, gallstones, and hernias may arise. Understanding the potential risks and complications is crucial in making an informed decision.
Lifestyle Changes and Commitment
Weight loss surgery is not a magic solution. It requires a commitment to significant lifestyle changes, including adopting a healthy and balanced diet, engaging in regular physical activity, and attending follow-up appointments. Patients must be willing to make these changes to achieve long-term success.
Benefits of Weight Loss Surgery
Significant and Sustained Weight Loss
Weight loss surgery has been proven to provide significant and sustained weight loss for individuals struggling with obesity. Many patients experience improvements in overall health, including reduced blood sugar levels, improved cholesterol profiles, and decreased blood pressure.
- Resolution of Obesity-related Health Conditions
- Weight loss surgery often leadsBenefits of Weight Loss Surgery (continued)
Resolution of Obesity-related Health Conditions
Weight loss surgery often leads to the resolution or improvement of obesity-related health conditions. Many individuals with type 2 diabetes, sleep apnea, and high blood pressure experience significant improvement or complete remission after undergoing weight loss surgery. This not only enhances their quality of life but also reduces the need for long-term medication.
Enhanced Mental and Emotional Well-being
Obesity can take a toll on an individual’s mental and emotional well-being, leading to low self-esteem, depression, and anxiety. Weight loss surgery can contribute to improved mental health by boosting self-confidence and body image. Patients often report increased energy levels, better moods, and an overall positive outlook on life.
Choosing the Best Weight Loss Surgery for You
When it comes to selecting the most suitable weight loss surgery, there is no one-size-fits-all approach. The decision should be based on individual factors, including medical history, current health conditions, weight loss goals, and the advice of a qualified healthcare professional. It is essential to have a thorough discussion with your healthcare team to determine which weight loss surgery option aligns best with your needs and preferences.
Factors to Consider When Choosing a Weight Loss Surgery
Weight Loss Goals and Expectations Consider your weight loss goals and expectations. Some weight loss surgeries may lead to more significant weight loss than others. Discuss your desired outcomes with your healthcare provider to ensure realistic expectations are set.
Health Conditions and Medical History
Evaluate your current health conditions and medical history. Certain weight loss surgeries may be more suitable for individuals with specific health concerns. It is important to disclose all relevant information to your healthcare team to make an informed decision.
Lifestyle and Commitment
Assess your lifestyle and commitment level. Different weight loss surgeries require varying degrees of lifestyle changes and long-term commitment. Understand the dietary and physical activity modifications necessary for each procedure and determine which one aligns with your ability to adopt and sustain those changes.
You may be wondering what type of weight loss surgery is best for your body. There are several different options to consider including Gastric bypass, Sleeve gastrectomy, Intragastric balloon, and Transarterial embolization.
The following article will help you choose which option is best for your body. You may also be interested in learning more about the pros and cons of each procedure. The following is a comparison of the two most common surgeries.
Gastric bypass
The Gastric Bypass is the best weight loss surgery for the body. It removes a large portion of the stomach and creates a small tube that holds the remaining contents. This surgery allows the body to feel full faster, as the stomach no longer contains as much food as it did before.
The surgery also improves insulin resistance, since the stomach no longer produces the hormone that triggers hunger. The surgery is permanent and cannot be reversed. The Roux-en-Y gastric bypass is the gold standard of weight loss surgery.
This procedure reduces the size of the upper stomach and limits the amount of food the body can absorb. The food bypasses the duodenum and the upper part of the small intestine. This helps reduce fat, calories, and the absorption of vitamins and minerals. Patients will lose a significant amount of weight, but their bodies will still be affected by the procedure.
Sleeve gastrectomy
If you’re overweight and not happy with your eating habits, Sleeve gastrectomy surgery may be the perfect option for you. The procedure involves cutting off the upper portion of the stomach, allowing you to eat less and maintain a healthy weight.
It can help you lose as much as 60% of your excess weight in just two years. A Sleeve gastrectomy will require regular medical checkups and dietary recommendations, but the results can be long-lasting. After the procedure, you will likely be released from the hospital after an hour or two.
In the days following surgery, you will be placed on a liquid diet, and you will gradually be allowed to eat small amounts of food. Following your recovery, you should avoid consuming large quantities of food for the first few days, as this can cause pain and discomfort.
The surgery is minimally invasive, and most patients can return to work within one to two weeks, although you will need to modify your activities for the first few weeks.
The first question that may arise in your mind is whether an intragastric balloon is the right weight loss surgery for you. If you have undergone bariatric surgery before, this procedure may not be right for you.
It can also affect your health if you have an inflammatory bowel disease. Other disqualifying factors for the surgery include a gastric mass or a hiatal hernia.
Intragastric balloon weight loss surgery results in an average loss of 60 to 70 percent of body weight, which has a positive impact on obesity-related diseases.
Patients undergoing gastric balloon surgery usually lose about 10 to 15 percent of their body weight during the first six months after the procedure. However, the results are not as dramatic as with gastric sleeve surgery.
Furthermore, you must commit to a 12-month exercise and diet program after the surgery. You may also be required to undergo a behavioral therapy program to enhance your weight loss.
Transarterial embolization
Transarterial embolization is an image-guided procedure that targets the endocrine function of the gastric fundus, a part of the gastric wall that is responsible for controlling appetite. This new method of weight loss surgery has seen promising preliminary results in adults suffering from severe obesity.
It reduces excess body weight by up to 11% and causes up to 7.6 kilograms of weight loss in 20 patients. In the initial phase of the study, eight participants had minor adverse events. The ideal agent for LGAE is unclear, but it does reduce the options for established surgical bariatric procedures.
For example, volume reduction in the devascularised area of the stomach may be ineffective, and in some cases, surgery might be ruled out altogether. In some cases, a gastric banding procedure may be the only option for those patients who have failed to lose weight despite multiple attempts that have proven unsuccessful.
Transarterial sleeve gastrectomy
A sleeve gastrectomy is a surgical procedure that involves the removal of a portion of the stomach. The surgeon creates a narrow sleeve in the stomach by vertically stapling the abdominal wall and removing the larger, curved part of the stomach.
The procedure can take one to two hours. After undergoing surgery, patients typically spend one to two nights in a hospital. Afterward, they are awakened in a recovery room. A doctor will place small surgical tools, including a laparoscope, through a series of tiny incisions in the upper abdomen.
A sleeve gastrectomy is a surgical procedure that reduces weight by removing part of the stomach. By removing part of the stomach, the amount of ghrelin, also known as the “hunger hormone,” will decrease.
The patient’s insulin level will likely decrease immediately and they may no longer require medications to control their diabetes. While the procedure is generally safe, there are potential risks and complications.
Frequently Asked Questions
1 How long does it take to recover from weight loss surgery?
Recovery time can vary depending on the type of weight loss surgery. Generally, patients can expect a recovery period of several weeks before resuming normal activities.
2 Will I have to follow a specific diet after weight loss surgery?
Yes, dietary changes are a crucial aspect of successful weight loss surgery. Your healthcare team will provide you with a detailed post-surgery diet plan to follow.
2 Is weight loss surgery covered by insurance?
In some cases, weight loss surgery may be covered by insurance if certain criteria are met. It is advisable to contact your insurance provider to understand your coverage options.
3 Can weight loss surgery be reversed?
While some weight loss surgeries are reversible, others are considered permanent. It is important to discuss the reversibility aspect with your healthcare provider before undergoing any procedure.
4 Will I need to take supplements after weight loss surgery?
Supplements may be recommended to ensure adequate nutrient intake after weight loss surgery. Your healthcare team will guide you on the specific supplements you may need.
5 Are there any age restrictions for weight loss surgery?
Age restrictions may vary depending on the type of weight loss surgery and individual circumstances. Your healthcare team will evaluate your overall health and determine if you are a suitable candidate for weight loss surgery.
6 Can I get pregnant after weight loss surgery?
Weight loss surgery can affect fertility, but it is possible to get pregnant after the procedure. It is important to discuss family planning with your healthcare provider and ensure proper nutrition and monitoring during pregnancy.
7 What are the potential risks of weight loss surgery?
Weight loss surgery carries risks, including infection, bleeding, blood clots, and complications related to anesthesia. Long-term risks may include nutritional deficiencies and the development of gallstones. Your healthcare team will discuss these risks with you before the surgery.
8 How long does it take to see results after weight loss surgery?
Weight loss results vary among individuals and depend on factors such as the type of surgery, adherence to dietary guidelines, and lifestyle changes. Some individuals may experience significant weight loss within the first few months, while others may have a more gradual progression.
9 Will I need to attend support groups after weight loss surgery?
Joining a support group can be beneficial for individuals who have undergone weight loss surgery. These groups provide a supportive environment to share experiences, exchange advice, and receive emotional support throughout the weight loss journey.
Remember, the decision to undergo weight loss surgery should be made after careful consideration and consultation with healthcare professionals. Each individual’s circumstances are unique, and what works for one person may not be the best option for another.
By understanding the different types of weight loss surgeries available, and the associated benefits, risks, and considerations, you can make an informed choice that aligns with your goals and promotes your overall well-being.
Conclusion
Weight loss surgery can be a life-changing solution for individuals struggling with obesity. By understanding the different types of weight loss surgeries available, their benefits, risks, and considerations, you can make an informed decision about the best option for your body. Remember to consult with a qualified healthcare professional who specializes in bariatric surgery to assess your eligibility, address any concerns, and guide you through the process.
Health
Understanding the Risk Factors for Developing Preeclampsia
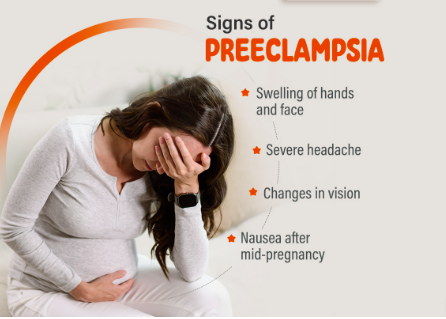
Understanding the Risk Factors for Developing Preeclampsia
Preeclampsia is a serious pregnancy complication characterized by high blood pressure and potential damage to organs such as the liver and kidneys.
It usually occurs after the 20th week of pregnancy and can have significant implications for both the mother and the baby.
Identifying the risk factors associated with preeclampsia is crucial for early intervention and management.
This article delves into the various risk factors, how they contribute to the development of preeclampsia and strategies for monitoring and prevention.
What Is Preeclampsia?
Preeclampsia is a condition that affects approximately 5-8% of pregnancies worldwide. It typically manifests with elevated blood pressure and proteinuria (excess protein in the urine).
If left untreated, it can lead to severe complications such as eclampsia, which involves seizures and can jeopardize both maternal and fetal health.
Risk Factors for Preeclampsia
Understanding the risk factors for preeclampsia can help in early diagnosis and management. Below are the primary risk factors associated with this condition:
1. Previous History of Preeclampsia
Women who have experienced preeclampsia in previous pregnancies are at a higher risk of developing the condition in subsequent pregnancies. The recurrence risk is approximately 20-30% if preeclampsia occurs in a previous pregnancy.
2. First Pregnancy
The risk of preeclampsia is higher in women who are pregnant for the first time. This is thought to be related to the body’s adjustment to the physiological changes associated with pregnancy.
3. Advanced Maternal Age
Women who are over the age of 35 are more likely to develop preeclampsia. The increased risk is associated with age-related changes in blood vessels and the body’s ability to manage pregnancy-related stress.
4. Multiple Gestations
Carrying more than one baby (e.g., twins or triplets) increases the risk of preeclampsia. The body’s increased demands and altered placental development contribute to this heightened risk.
5. Obesity
Obesity is a significant risk factor for preeclampsia. Excess body weight can lead to increased blood pressure and insulin resistance, both of which are associated with a higher likelihood of developing preeclampsia.
6. Chronic Hypertension
Women with pre-existing high blood pressure are at a greater risk of developing preeclampsia. Chronic hypertension can exacerbate the blood pressure problems associated with preeclampsia.
7. Diabetes
Both type 1 and type 2 diabetes are associated with an increased risk of preeclampsia. Diabetes can affect blood vessel function and increase the likelihood of high blood pressure during pregnancy.
8. Kidney Disease
Pre-existing kidney conditions can elevate the risk of preeclampsia. The kidneys play a crucial role in managing blood pressure and fluid balance, and any pre-existing conditions can compromise their function.
9. Autoimmune Disorders
Certain autoimmune disorders, such as lupus and rheumatoid arthritis, can increase the risk of developing preeclampsia. These conditions can affect the body’s immune response and vascular health.
10. Family History
A family history of preeclampsia can indicate a genetic predisposition to the condition. Women with a family history are at an increased risk compared to those without such a history.
11. Poor Nutrition
Inadequate nutrition, particularly a lack of essential vitamins and minerals such as calcium and magnesium, can contribute to the development of preeclampsia. Proper prenatal care and nutrition are crucial for minimizing risk.
12. Infections
Certain infections during pregnancy, such as urinary tract infections, can be associated with an increased risk of preeclampsia. Infections can exacerbate the inflammatory processes involved in preeclampsia.
13. High Stress Levels
Chronic stress and poor mental health can impact overall well-being and contribute to conditions like preeclampsia. Managing stress through healthy lifestyle choices and support systems is important.
Monitoring and Prevention Strategies
Early monitoring and preventive measures can help manage the risk factors associated with preeclampsia:
- Regular Prenatal Visits: Frequent check-ups with a healthcare provider can help monitor blood pressure and other indicators of preeclampsia.
- Healthy Lifestyle Choices: Maintaining a balanced diet, engaging in regular physical activity, and managing weight can reduce the risk.
- Medication: In some cases, medications such as aspirin may be recommended to lower the risk of preeclampsia, especially for women with a high risk.
- Stress Management: Techniques such as mindfulness, relaxation exercises, and counseling can help manage stress and support overall health.
- Education and Awareness: Understanding the symptoms and risk factors of preeclampsia can help in early detection and timely intervention.
Conclusion
Preeclampsia is a complex condition with multiple risk factors. By recognizing these factors and taking proactive steps, expectant mothers can work with their healthcare providers to manage their risk and promote a healthier pregnancy.
Regular prenatal care, lifestyle modifications, and stress management are key to minimizing the impact of preeclampsia and ensuring the best possible outcomes for both mother and baby.
FAQs
1. What are the early signs of preeclampsia?
Early signs of preeclampsia include high blood pressure, proteinuria, swelling of the hands and feet, sudden weight gain, and severe headaches. It’s important to report any unusual symptoms to your healthcare provider promptly.
2. Can preeclampsia be prevented?
While not all cases of preeclampsia can be prevented, maintaining a healthy lifestyle, attending regular prenatal visits, and following your healthcare provider’s recommendations can help reduce the risk.
3. How is preeclampsia diagnosed?
Preeclampsia is diagnosed through routine prenatal screenings that monitor blood pressure and urine protein levels. If preeclampsia is suspected, additional tests may be conducted to assess kidney function and other health indicators.
4. What are the treatment options for preeclampsia?
Treatment options for preeclampsia depend on the severity of the condition. They may include medications to manage blood pressure, bed rest, and in severe cases, early delivery of the baby to protect both the mother and child.
5. Can preeclampsia affect future pregnancies?
Having preeclampsia in one pregnancy can increase the risk of developing it in future pregnancies. However, many women go on to have healthy pregnancies by managing risk factors and following their healthcare provider’s advice.
References:
Health
Top 5 Immunity-Boosting Fruits to Include in Your Diet

Top 5 Immunity-Boosting Fruits to Include in Your Diet
In our quest for better health, the immune system often takes center stage. One of the simplest and most effective ways to support this vital system is through a nutritious diet.
Fruits, rich in essential vitamins, minerals, and antioxidants, can play a significant role in strengthening your immune system.
In this article, we’ll explore the best fruits for boosting immunity, backed by scientific research, and provide practical tips for incorporating them into your daily routine.
Why Immune Health Matters
The immune system is our body’s defense mechanism against harmful pathogens, including bacteria, viruses, and toxins.
A robust immune system can help fend off illnesses and infections, and a balanced diet is crucial for maintaining its optimal function.
Fruits, in particular, offer a wealth of nutrients that can enhance immune response, improve overall health, and even prevent chronic diseases.
1. Citrus Fruits: Vitamin C Powerhouses
Oranges
Oranges are synonymous with vitamin C, a crucial nutrient for immune health. Vitamin C supports the production and function of white blood cells, which are essential for fighting infections.
Just one medium-sized orange provides about 70 mg of vitamin C, meeting the daily recommended intake for most adults.
Grapefruits
Grapefruits, another excellent source of vitamin C, also contain antioxidants like lycopene, which have been linked to reduced inflammation and improved immune function.
Enjoying half a grapefruit a day can contribute significantly to your vitamin C needs.
Lemons
Lemons are versatile fruits that not only boost your vitamin C intake but also support detoxification.
Adding lemon juice to water or dishes can enhance your immune system while providing a refreshing flavor.
2. Berries: Antioxidant-Rich Superfoods
Blueberries
Blueberries are packed with antioxidants, particularly flavonoids, which help combat oxidative stress and inflammation.
These antioxidants can enhance immune function and protect against chronic diseases. A cup of fresh blueberries is a delicious way to boost your immunity.
Strawberries
Strawberries are another berry with a high vitamin C content, along with various antioxidants that contribute to overall health.
A handful of strawberries can provide a significant portion of your daily vitamin C requirement.
Raspberries
Raspberries are rich in vitamins C and E, as well as fiber and antioxidants.
These nutrients work together to support immune health and maintain digestive well-being.
Incorporate raspberries into smoothies or salads for a tasty immune boost.
4. Papaya
Papaya is an excellent source of vitamin C, vitamin A, and digestive enzymes such as papain. These nutrients contribute to a stronger immune system by supporting cellular repair and reducing inflammation.
5. Pomegranate
Pomegranates are rich in antioxidants and vitamin C, which help combat oxidative stress and boost immune function. The anti-inflammatory properties of pomegranates also support overall health and wellness.
Incorporating these fruits into your daily diet can provide essential nutrients that support immune health and help protect your body against illnesses.
Frequently Asked Questions
1. How does vitamin C boost the immune system?
Vitamin C enhances the production of white blood cells, which are crucial for combating infections and illnesses. It also acts as an antioxidant, protecting cells from damage caused by free radicals.
2. Can berries help reduce inflammation?
Yes, berries are rich in antioxidants and vitamins that help reduce inflammation and oxidative stress, which can support overall immune function.
3. What are the benefits of kiwi for immune health?
Kiwi provide a high amount of vitamin C, which supports the immune system by increasing white blood cell production. It also contains vitamin K and folate, which are essential for maintaining overall health.
4. How does papaya contribute to immune health?
Papaya is high in vitamin C and vitamin A, which help strengthen the immune system. Additionally, the enzyme papain in papaya aids in digestion and reduces inflammation.
5. What makes pomegranates beneficial for immunity?
Pomegranates are rich in antioxidants and vitamin C, which help fight oxidative stress and inflammation, thereby supporting the immune system and overall health.
References:
Healthline – Best Fruits for Boosting Immunity
Health
Effective Medications to Lower Cholesterol: A Comprehensive Guide

Effective Medications to Lower Cholesterol: A Comprehensive Guide
High cholesterol is a common health issue that can significantly increase the risk of heart disease, stroke, and other serious health conditions. Fortunately, various medications are available to help manage and lower cholesterol levels.
In this guide, we’ll explore the most effective medications for lowering cholesterol, their mechanisms of action, potential side effects, and other crucial information to help you make informed decisions about your health.
Understanding Cholesterol and Its Impact on Health
Cholesterol is a fatty substance found in your blood. Your body needs cholesterol to build healthy cells, but having high levels of cholesterol can increase your risk of heart disease.
Cholesterol travels through your bloodstream in two main types of lipoproteins:
low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
- LDL Cholesterol: Often referred to as “bad” cholesterol, LDL can build up in the walls of your arteries, leading to atherosclerosis, which can restrict blood flow and increase the risk of heart attacks and strokes.
- HDL Cholesterol: Known as “good” cholesterol, HDL helps remove LDL cholesterol from your arteries, reducing the risk of cardiovascular problems.
Why Medication May Be Necessary
Even with a healthy diet and regular exercise, some individuals may still struggle to manage their cholesterol levels.
This is where cholesterol-lowering medications come into play. These medications work in various ways to help lower LDL cholesterol and, in some cases, raise HDL cholesterol.
Types of Cholesterol-Lowering Medications
1. Statins
Statins are the most commonly prescribed medications for lowering LDL cholesterol.
They work by blocking a substance your body needs to make cholesterol, thus reducing the amount of LDL cholesterol in your bloodstream.
- Examples: Atorvastatin (Lipitor), Simvastatin (Zocor), Rosuvastatin (Crestor)
- Mechanism of Action: Statins inhibit the enzyme HMG-CoA reductase, which is involved in cholesterol production in the liver.
- Common Side Effects: Muscle pain, digestive problems, increased liver enzymes
- Benefits: Statins are highly effective in reducing LDL cholesterol levels and have been shown to lower the risk of heart attacks and strokes.
2. Bile Acid Sequestrants
Bile acid sequestrants work by binding to bile acids in the intestine, preventing them from being reabsorbed. This process forces the liver to use cholesterol to produce more bile acids, thus lowering LDL cholesterol levels.
- Examples: Cholestyramine (Prevalite), Colestipol (Colestid), Colesevelam (Welchol)
- Mechanism of Action: These drugs bind bile acids in the intestines, reducing cholesterol absorption.
- Common Side Effects: Constipation, bloating, nausea
- Benefits: Effective at lowering LDL cholesterol and can be used in conjunction with statins for enhanced results.
3. Niacin
Niacin (also known as vitamin B3) helps lower LDL cholesterol and raise HDL cholesterol levels.
It works by decreasing the liver’s production of LDL cholesterol and increasing HDL cholesterol.
- Examples: Niacor, Niaspan
- Mechanism of Action: Niacin reduces the production of LDL cholesterol and increases HDL cholesterol.
- Common Side Effects: Flushing, itching, liver damage (with high doses)
- Benefits: Effective in raising HDL cholesterol and lowering LDL cholesterol.
4. Fibric Acids
Fabric acids, or fibrates, are primarily used to lower triglyceride levels and can also help increase HDL cholesterol levels.
They work by activating a protein that helps break down triglycerides in the blood.
- Examples: Fenofibrate (Tricor), Gemfibrozil (Lopid)
- Mechanism of Action: They activate peroxisome proliferator-activated receptors (PPARs), which help in the breakdown of triglycerides.
- Common Side Effects: Muscle pain, liver abnormalities, gastrointestinal issues
- Benefits: Particularly useful for individuals with high triglyceride levels.
5. PCSK9 Inhibitors
PCSK9 inhibitors are a newer class of cholesterol-lowering medications that help the liver remove LDL cholesterol from the bloodstream more effectively.
- Examples: Alirocumab (Praluent), Evolocumab (Repatha)
- Mechanism of Action: These drugs inhibit the PCSK9 protein, which normally reduces the liver’s ability to remove LDL cholesterol from the blood.
- Common Side Effects: Injection site reactions, flu-like symptoms
- Benefits: Very effective at lowering LDL cholesterol, especially in individuals who cannot tolerate statins.
6. Cholesterol Absorption Inhibitors
Cholesterol absorption inhibitors work by blocking the absorption of cholesterol from the diet, which reduces the amount of cholesterol that enters your bloodstream.
- Examples: Ezetimibe (Zetia)
- Mechanism of Action: They inhibit the absorption of cholesterol in the small intestine.
- Common Side Effects: Diarrhea, stomach pain, muscle pain
- Benefits: Can be used alone or in combination with statins to lower LDL cholesterol.
Choosing the Right Medication
The choice of medication depends on various factors, including your overall health, the specific cholesterol issue you have, and how well you tolerate certain medications.
Your healthcare provider will help you determine the most appropriate medication based on your individual needs and medical history.
Lifestyle Modifications to Complement Medication
While medications are effective in managing cholesterol levels, they work best when combined with lifestyle changes.
Consider incorporating the following into your routine:
- Healthy Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins while avoiding saturated fats and trans fats.
- Regular Exercise: Engage in at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week.
- Weight Management: Achieve and maintain a healthy weight to help control cholesterol levels.
- Avoid Smoking and Limit Alcohol: Both smoking and excessive alcohol intake can negatively impact cholesterol levels.
Monitoring and Follow-Up
Regular follow-up with your healthcare provider is crucial to monitor your cholesterol levels and assess the effectiveness of your medication. Your doctor may adjust your treatment plan based on your progress and any side effects you experience.
Final Thoughts
Managing cholesterol is a critical aspect of maintaining cardiovascular health.
With a variety of effective medications available, it’s possible to lower LDL cholesterol levels and reduce the risk of heart disease and other complications.
However, medication alone is not a cure-all; combining it with lifestyle changes is essential for optimal results.
Always consult your healthcare provider for personalized advice and treatment plans tailored to your specific needs.
Frequently Asked Questions (FAQs)
1. What is the primary goal of cholesterol-lowering medications?
Cholesterol-lowering medications primarily aim to reduce LDL cholesterol levels in the blood, thereby decreasing the risk of cardiovascular diseases such as heart attacks and strokes.
2. Are there any natural alternatives to cholesterol-lowering medications?
Yes, some natural alternatives include dietary changes (e.g., increased intake of soluble fiber and omega-3 fatty acids), regular exercise, and weight management. However, these should be used in conjunction with, not as a replacement for, prescribed medications.
3. How long does it take for cholesterol-lowering medications to show results?
The effects of cholesterol-lowering medications can usually be observed within a few weeks, but it may take several months to see significant changes in cholesterol levels and overall cardiovascular risk.
4. Can cholesterol-lowering medications cause side effects?
Yes, some common side effects include muscle pain, digestive issues, and liver enzyme changes. It’s important to report any side effects to your healthcare provider for proper management.
5. Can I stop taking my cholesterol medication if my levels improve?
It’s important to consult your healthcare provider before making any changes to your medication regimen. Discontinuing medication without medical advice can lead to a rebound in cholesterol levels and an increased risk of heart disease.
References
Cholesterol-lowering Medications
-

 Trending Stories1 year ago
Trending Stories1 year agoCDC: 1 in 4 Americans Still COVID-Free by End of 2022
-

 Health5 years ago
Health5 years agoMeghan Trainor Shares Motivational New Song ‘Blink’
-

 Health2 years ago
Health2 years agoHow Long Does Monkey Pox Last Before It Surfaces in the Body?
-

 Health2 years ago
Health2 years agoWhat Causes Swollen Body? Understanding Edema and its Triggers
-

 Health3 years ago
Health3 years agoNutrition and the Importance of a Fitness Program – 3 Things to Know
-

 Health3 years ago
Health3 years ago5 Weird Reasons Why Pimples Disappear After Marriage
-

 Health3 months ago
Health3 months agoHow Do Pawpaw Seeds Support Cardiovascular Health?
-

 Health2 years ago
Health2 years agoHealth Benefits Of Pawpaw Seed? 7 Things To Know





