Health
Are Yellow Fever Vaccines Covered by Health Insurance?

Are Yellow Fever Vaccines Covered by Health Insurance?
In the ever-growing world of health insurance, it can be hard to keep up with what’s covered and what’s not.
That’s why we’ve compiled a comprehensive list of all the important information you need to know about yellow fever vaccines and whether or not they’re covered by your health insurance.
We’ll also tell you how to make an appointment to receive your vaccine at Campus Health, as well as answer any questions you may have about the vaccine itself.
So whether you’re in the US or another country that requires yellow fever vaccination, make sure you read this blog before making any decisions!
Are yellow fever vaccines covered by insurance?

Are yellow fever vaccines covered by insurance? This question is on the minds of many people these days, as the mosquito-borne disease has made a comeback in recent years.
While there is no specific vaccine for yellow fever, coverage may vary depending on your health insurance plan.
If you are unable to get vaccinated because it isn’t covered by your insurance, consider a preventative
measure like wearing insect repellent and staying indoors during peak hours of the mosquito season.
Vaccination against yellow fever is highly effective and is one of the most important things you can do to protect yourself and your loved ones.
So make sure to check with your insurer before getting vaccinated, and don’t skip this life-saving vaccine!
Which countries require yellow fever vaccines?

When it comes to traveling, it’s always a good idea to be prepared for anything.
That’s why it’s important to know which countries require yellow fever vaccines.
This vaccine is necessary for travelers going to some areas in Africa or the Caribbean, and depending on the country, vaccination may be mandatory for all travelers aged 9 months and older.
If you’re traveling to one of these countries and have the required paperwork (proof of vaccination), getting vaccinated should not cause any issues with your health insurance coverage!
However, it’s always a good idea to speak with an expert before making any travel decisions, just in case there are any exclusions or restrictions on which vaccines you need.
So pack your vaccines, lock your doors, and hit the road – you’re about to embark on an amazing journey!
How much does Yellow Fever Vaccine cost?

Are you planning a trip to a country where yellow fever is present? If so, you should get vaccinated against the disease.
Many people are unaware that yellow fever vaccines are covered by their health insurance. So, before booking your appointment or getting vaccinated, make sure to check with your insurance company.
The cost of the vaccine can vary depending on your province or state, but it’s usually very affordable.
Make sure you get vaccinated against yellow fever before you travel, as it’s an effective disease and can be deadly if not treated properly.
what are the symptoms of yellow fever
If you are traveling to an area where yellow fever is present, it is essential that you get vaccinated.
The vaccine is safe and most people who receive it do not experience any side effects.
Vaccination is usually covered by your health insurance, so make sure to ask your insurer about coverage before traveling.
Is There a Treatment or Cure for Yellow Fever?
There is no cure for yellow fever, but there is a treatment available that can help prolong your life.
The vaccine will give you immunity to the virus, so you won’t get sick if you are exposed to it. Most health insurance companies now cover the cost of yellow fever vaccines. So if you are traveling to
an area where the virus is prevalent, make sure to get vaccinated against it as soon as possible!
Who Should Get the Yellow Fever Vaccine?
Anyone who lives or works in any of the countries listed below should get vaccinated against yellow fever, as there is a risk of contracting the disease while traveling to these areas:
– Argentina – Bolivia – Brazil – Chile – Colombia – Ecuador Peru Venezuela (excluding Puerto Rico) + Angola, Benin, Burkina Faso, Chad, Congo DRC (Republic of), Cote d’Ivoire (Ivory Coast), Gambia, Ghana, Guinea Bissau, Liberia, Mali Mauritania Niger Nigeria Senegal Sierra Leone Solomon Islands Togo Uganda.
There is currently no vaccine available for those traveling to the US (). The yellow fever vaccine is available free of charge to all citizens of most countries and health insurance providers usually cover it.
Check with your provider first before getting vaccinated.
How do I make an appointment to receive the Yellow Fever Vaccine at Campus Health?

Are you worried about the Yellow Fever pandemic? Campus Health can help you find out if your health insurance covers the vaccine and make an appointment for you to receive it.
You will need to bring proof of coverage with you, such as your policy book or card.
However, the vaccine is not usually covered by most health insurance plans.
If you do find out that your health insurance does cover the vaccine, be sure to bring it with you to the appointment so that you can get it.
In the meantime, make sure you are up-to-date on the latest information about the pandemic by checking out our website or social media pages.
What if I only need a Yellow Fever Card replaced?
 It’s important to be up to date on vaccinations for the upcoming season. This includes vaccination against yellow fever.
It’s important to be up to date on vaccinations for the upcoming season. This includes vaccination against yellow fever.
Depending on your health insurance, it may cover the cost of a yellow fever vaccine.
Make sure to keep an eye on announcements from the health authorities in order to be aware of any changes that may affect vaccinations.
Additionally, always confirm with your doctor that a yellow fever vaccine is necessary before traveling.
Frequently Asked Questions
Which vaccine should I get, if I’m age 6 months or older and living in an area where yellow fever is a risk?
If you are age 6 months or older, and reside in an area where yellow fever is a risk, there is no wrong answer when it comes to which vaccine you should get. However, some of the most common vaccines that provide protection against yellow fever include the measles, mumps, rubella (MMR) vaccine and varicella (chickenpox) vaccine. So, whichever one you choose, make sure to get it!
When is the Yellow Fever season in the US?
The yellow fever season in the US typically runs from around May to October. It’s typically found in areas around the world where mosquitoes that carry the virus are present. For example, yellow fever can be found in parts of Africa, South, and Central America, Asia, and the Caribbean. The vaccine against yellow fever is available through most health insurance plans in the US. So, if you’re traveling to one of these areas and are concerned about becoming ill with yellow fever, make sure to get vaccinated before you go.
What are the symptoms of yellow fever?
If you are in a yellow fever risk area, such as South America or Africa, it is highly recommended that you get vaccinated against the disease. Vaccination offers long-term protection against yellow fever and avoids many complications that may arise from its contraction. The most common symptoms of yellow fever are high fever, jaundice (yellowing of the skin and eyes), rash, and muscle aches.
What if I am pregnant or have a severe disability that prevents me from traveling to an area where yellow fever is a risk?
If you are pregnant or have a severe disability that prevents you from traveling to an area where yellow fever is a risk, you may be able to get a waiver to exempt yourself from vaccinating. You can also research health insurance companies and find out if they cover vaccines for yellow fever in cases like this.
How do I find out if my health insurance covers yellow fever vaccines?
To find out if your health insurance covers yellow fever vaccines, you can call their customer service line. There are also some third-party resources like the Immunization Action Coalition (IAC) and HealthMap that can help in finding out if your health insurer offers yellow fever vaccine exemptions. If you’re not sure, another option is to look online for a list of health insurance providers that cover vaccines.
Conclusion
The short answer is that yellow fever vaccines are not typically covered by health insurance, but there are some exceptions. Make sure to check with your insurance provider to see if yellow fever vaccines are covered and if you have any pre-existing health conditions that might affect the vaccine’s effectiveness. In the meantime, Campus Health offers free vaccination clinics every semester for students to receive the yellow fever vaccine. Check our website for more information or call us at 925.762.2222 for an appointment.
Health
Iowa Reports First Fatal Case of Ebola-like Lassa Fever Following Travel to West Africa

Iowa Reports First Fatal Case of Ebola-like Lassa Fever Following Travel to West Africa
Iowa health officials recently confirmed a fatal case of Lassa fever, an Ebola-like viral disease, in a person who had recently traveled to West Africa.
This incident has raised concerns about Lassa fever’s risks, transmission methods, and potential impacts on public health, especially as it is one of the few recorded cases of this virus in the United States.
This article will provide an in-depth overview of Lassa fever, its origins, symptoms, transmission risks, and the measures people can take to protect themselves and those around them.
Understanding Lassa Fever
What is Lassa Fever?
Lassa fever is a hemorrhagic virus similar in presentation to Ebola, transmitted primarily by contact with food or objects contaminated with infected rodent urine or feces.
This viral disease is common in parts of West Africa, where an estimated 100,000 to 300,000 cases are reported annually. Though many cases go unreported, the virus can cause severe illness and death in severe cases, particularly in patients with underlying health conditions.
Lassa Fever vs. Ebola: What’s the Difference?
Both Lassa fever and Ebola are viral hemorrhagic fevers, but they differ in their method of transmission, symptom severity, and geographical reach.
While Ebola spreads through human-to-human contact, Lassa fever is mainly rodent-borne and spread through direct or indirect exposure to rodents’ excretions.
Ebola outbreaks have historically shown higher fatality rates, but Lassa fever is often underreported, making mortality comparisons challenging.
Origins and Transmission of Lassa Fever
Where Does Lassa Fever Come From?
Lassa fever was first identified in 1969 in Nigeria and has since remained endemic in countries like Sierra Leone, Liberia, Guinea, and Nigeria.
The Mastomys rat, or “multimammate rat,” serves as the natural reservoir for the virus and is a common species in West African regions, leading to frequent human contact and possible transmission.
How is Lassa Fever Transmitted?
Transmission occurs mainly through:
- Direct contact with infected rodents’ urine or droppings.
- Ingestion of contaminated food or household items.
- Human-to-human transmission in healthcare settings due to improper hygiene practices or exposure to bodily fluids of infected individuals.
The virus does not spread through casual contact, making general public spread less likely unless in close contact with contaminated surfaces or bodily fluids.
Symptoms of Lassa Fever
Early Symptoms
Early symptoms of Lassa fever can be mild, leading to undiagnosed cases or delayed medical attention.
Symptoms typically appear 1-3 weeks after exposure and may include:
- Fever and fatigue
- Sore throat and cough
- Nausea, vomiting, and diarrhea
- Abdominal and chest pain
Severe Symptoms and Complications
As the disease progresses, patients may develop more severe symptoms like:
- Hemorrhaging from gums, eyes, or nose
- Facial swelling and fluid in the lungs
- Seizures and confusion
- Organ failure
While some patients recover within weeks, severe complications can arise, especially in pregnant women and individuals with preexisting health conditions.
Diagnosis and Treatment
How is Lassa Fever Diagnosed?
Diagnosis requires specialized laboratory testing, as Lassa fever’s early symptoms resemble many other viral illnesses.
Polymerase chain reaction (PCR) tests and ELISA (enzyme-linked immunosorbent assay) can identify viral RNA and antibodies in blood samples, aiding in accurate diagnosis.
Treatment Options
Antiviral medication, such as ribavirin, has shown promise in reducing symptoms when administered early. Supportive care, including rehydration, oxygen therapy, and blood transfusions, is crucial for severe cases.
However, there is no universally approved vaccine, making prevention through hygiene and rodent control vital.
Preventive Measures for Lassa Fever
Minimizing Contact with Rodents
Effective rodent control is essential in areas where Lassa fever is prevalent. Keeping food in rodent-proof containers, clearing homes of food scraps, and storing waste away from living spaces can minimize exposure to rodent excretions.
Maintaining Hygiene in Healthcare Settings
In hospitals, isolation protocols and rigorous hygiene practices, including the use of gloves, masks, and proper disposal of waste, are critical to prevent transmission from infected individuals to healthcare workers or family members.
Public Health Concerns and Global Impact
Why Should We Be Concerned About Lassa Fever?
While cases outside of West Africa are rare, the recent case in Iowa illustrates the potential for Lassa fever to appear in non-endemic regions.
Increased global travel poses risks, necessitating enhanced screening and awareness, especially for travelers returning from high-risk areas.
The Role of the CDC and WHO
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) play significant roles in monitoring and controlling Lassa fever outbreaks.
Both organizations work closely with local health agencies to provide guidelines, support diagnosis, and enhance preventive measures.
Conclusion
The tragic loss of life due to Lassa fever in Iowa serves as a stark reminder of the potential dangers of hemorrhagic fevers. Increased awareness, hygiene measures, and public health vigilance are essential to prevent future cases and protect communities.
As international travel grows, so does the need for education on preventing and responding to rare but deadly diseases like Lassa fever.
Frequently Asked Questions (FAQs)
1. Can Lassa fever be spread through the air?
No, Lassa fever is not airborne. It spreads through contact with rodent excretions or bodily fluids of an infected person.
2. Is there a vaccine available for Lassa fever?
Currently, there is no FDA-approved vaccine for Lassa fever, though researchers are actively working on developing one.
3. What regions are considered high-risk for Lassa fever?
High-risk regions include West African countries such as Nigeria, Sierra Leone, Liberia, and Guinea, where the Mastomys rodent is prevalent.
4. What should travelers do to protect themselves from Lassa fever?
Travelers to endemic regions should avoid contact with rodents, keep food secured, and wash hands frequently. It’s wise to stay updated on health advisories from the CDC.
5. How can healthcare facilities prevent Lassa fever spread?
Hospitals can reduce risks by implementing stringent hygiene protocols, using personal protective equipment, and isolating infected patients to prevent cross-contamination.
References :
Health
Understanding Menstrual Allergy: What You Need to Know

Understanding Menstrual Allergy: What You Need to Know
REFERENCE:
https://www.healthwellnessjournal.com/menstrual-allergy-guide
Health
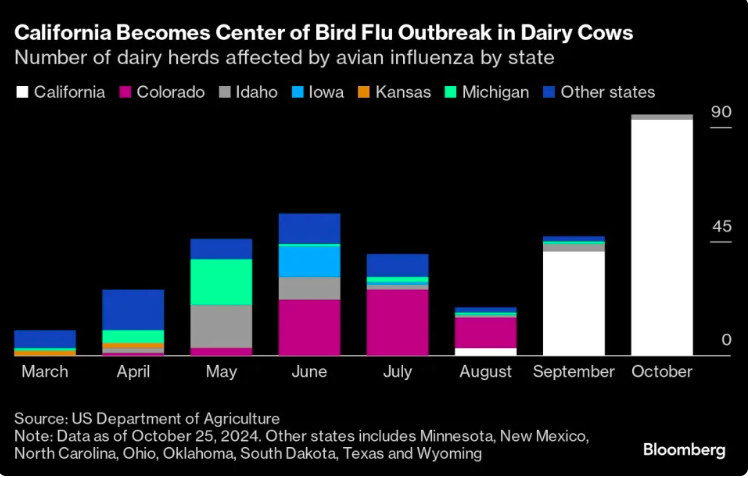
California’s Bird Flu Crisis in Cattle: Understanding the Threat to Farming and Public Health
-

 Trending Stories1 year ago
Trending Stories1 year agoCDC: 1 in 4 Americans Still COVID-Free by End of 2022
-

 Health5 years ago
Health5 years agoMeghan Trainor Shares Motivational New Song ‘Blink’
-

 Health7 months ago
Health7 months agoHow Do Pawpaw Seeds Support Cardiovascular Health?
-

 Health2 years ago
Health2 years agoHow Long Does Monkey Pox Last Before It Surfaces in the Body?
-

 Health3 years ago
Health3 years agoWhat Causes Swollen Body? Understanding Edema and its Triggers
-

 Health3 years ago
Health3 years agoNutrition and the Importance of a Fitness Program – 3 Things to Know
-

 Health3 years ago
Health3 years ago5 Weird Reasons Why Pimples Disappear After Marriage
-

 Health2 years ago
Health2 years agoHealth Benefits Of Pawpaw Seed? 7 Things To Know