Health
Understanding the Ten Causes of Malaria: Shedding Light on the Factors Behind the Disease

Understanding the Ten Causes of Malaria: Shedding Light on the Factors Behind the Disease
1. Mosquitoes: The primary cause of malaria is the female Anopheles mosquito. These mosquitoes are carriers of the Plasmodium parasite, which causes the disease. When an infected mosquito bites a human, it injects the parasite into the bloodstream, initiating the infection.
2. Plasmodium Parasite: Several species of the Plasmodium parasite can cause malaria in humans, with Plasmodium falciparum being the most deadly. Once inside the human body, the parasite multiplies and infects red blood cells, leading to the characteristic symptoms of malaria.
3. Lack of Effective Control Measures: In areas where malaria is endemic, the lack of effective control measures contributes to the high prevalence of the disease. Insufficient mosquito control strategies, such as the use of insecticide-treated bed nets and indoor residual spraying, allow mosquitoes to thrive and transmit the parasite.
4. Climate and Environmental Factors: Malaria transmission is greatly influenced by climate and environmental factors. Mosquitoes require specific temperature and humidity conditions to breed and survive. Therefore, regions with warm and humid climates provide an ideal environment for the proliferation of mosquitoes and the spread of malaria.
5. Poverty and Lack of Access to Healthcare: Malaria disproportionately affects populations living in poverty and those with limited access to healthcare. These individuals often lack the resources to protect themselves from mosquito bites and seek timely diagnosis and treatment, leading to higher rates of infection and mortality.
6. Travel and Migration: The movement of infected individuals from malaria-endemic areas to non-endemic regions plays a significant role in the global spread of the disease. Travelers and migrants can unknowingly carry the parasite with them, introducing it to new areas where the local population may have little to no immunity.
7. Drug Resistance: The emergence of drug-resistant strains of the Plasmodium parasite poses a serious challenge to malaria control efforts. Resistance to commonly used antimalarial drugs, such as chloroquine and sulfadoxine-pyrimethamine, reduces the effectiveness of treatment and increases the risk of complications and mortality.
8. Lack of Public Health Infrastructure: Inadequate public health infrastructure, particularly in resource-limited settings, hinders the prevention and control of malaria. Limited access to diagnostic tools, antimalarial medications, and healthcare facilities makes it difficult to diagnose and treat cases promptly, allowing the disease to persist.
9. Socioeconomic Factors: Social and economic factors, such as population displacement, urbanization, and deforestation, can contribute to the spread of malaria. These factors disrupt ecosystems, create new breeding grounds for mosquitoes, and increase human-mosquito contact, facilitating the transmission of the parasite.
10. Lack of Education and Awareness: Insufficient knowledge about malaria and its prevention among affected communities further exacerbates the problem. Without proper education and awareness campaigns, individuals may not understand the importance of using preventive measures or seeking early diagnosis and treatment, leading to continued transmission.
By understanding the ten primary causes of malaria, policymakers, healthcare providers, and communities can work together to develop comprehensive strategies that address these factors.
Efforts to control malaria require a multi-faceted approach that includes mosquito control, improved healthcare access, education, and research to develop new tools and interventions. Only through a concerted global effort can we hope to eliminate malaria and alleviate the burden it places on millions of people worldwide.
Mosquito-Borne Parasites
The main cause of malaria is the transmission of parasites from infected mosquitoes to humans. The most common malaria parasite is Plasmodium falciparum, responsible for the majority of malaria-related deaths worldwide. Other species of the parasite, such as Plasmodium vivax, Plasmodium malaria, and Plasmodium ovale, also contribute to the disease burden.
Prevention tip: Protect yourself from mosquito bites by using insect repellents, sleeping under mosquito nets, and wearing protective clothing.
Mosquito-borne diseases have been a significant public health concern for centuries. Malaria, caused by the transmission of parasites from infected mosquitoes to humans, is one of the most well-known and deadly mosquito-borne diseases.
The parasites responsible for malaria belong to the genus Plasmodium, with Plasmodium falciparum being the most prevalent and dangerous species. It is responsible for the majority of malaria-related deaths worldwide, particularly in sub-Saharan Africa.
However, other species of the Plasmodium parasite also contribute to the disease burden. Plasmodium vivax, for example, is the second most common species and is prevalent in Asia and Latin America. Plasmodium malaria and Plasmodium ovale are less common but can still cause malaria in humans.
To prevent mosquito-borne diseases like malaria, it is crucial to take preventive measures. Using insect repellents containing DEET or other approved ingredients can help repel mosquitoes and reduce the risk of bites.
Additionally, sleeping under mosquito nets, specially treated with insecticides, can provide an effective barrier against mosquito bites during sleep. Wearing protective clothing, such as long sleeves and pants, can also minimize exposure to mosquitoes, particularly in areas with high malaria transmission rates.
Anopheles Mosquitoes
Malaria is primarily transmitted by female Anopheles mosquitoes, which carry and transmit the malaria parasites. These mosquitoes thrive in warm and humid climates, making tropical and subtropical regions particularly susceptible to malaria outbreaks.
Prevention tip: Eliminate mosquito breeding sites by removing stagnant water sources and using insecticides to control mosquito populations.
Understanding the behavior and biology of Anopheles mosquitoes is crucial in combating malaria. These mosquitoes are most active during the night, with peak biting times occurring between dusk and dawn.
They are attracted to human hosts by the carbon dioxide we exhale, as well as by body heat and certain odors. Anopheles mosquitoes have a preference for biting indoors, seeking out dark and cool places to rest during the day.
Efforts to prevent malaria transmission involve a combination of strategies, including vector control measures. In addition to eliminating breeding sites and using insecticides, other approaches such as the use of bed nets treated with insecticides have proven effective in reducing mosquito bites and preventing malaria infections.
These bed nets create a physical barrier between humans and mosquitoes, preventing them from accessing their blood meal. Furthermore, research and development efforts have focused on finding innovative tools to combat malaria.
For example, scientists are exploring the use of genetically modified mosquitoes that are resistant to the malaria parasite or that have reduced lifespan, thus limiting their ability to transmit the disease.
This approach, known as genetic control, shows promise in reducing the population of malaria-transmitting mosquitoes and ultimately reducing the burden of malaria.
In conclusion, understanding the biology and behavior of Anopheles mosquitoes is crucial in preventing malaria transmission. By implementing comprehensive vector control measures and exploring innovative approaches, we can make significant progress in reducing the global burden of this devastating disease.
Travel to Malaria-Endemic Areas
Traveling to regions where malaria is endemic increases the risk of contracting the disease. Tourists and individuals visiting friends and relatives in malaria-endemic areas may have limited immunity and are more susceptible to infection.
Malaria is a serious disease caused by a parasite transmitted through the bite of infected mosquitoes. It is prevalent in tropical and subtropical regions, including parts of Africa, Asia, and the Americas.
Prevention tip: Seek advice from healthcare professionals before traveling to malaria-endemic areas. Take prophylactic medications as prescribed and follow preventive measures to reduce the risk of infection.
It is crucial to consult with a healthcare provider who specializes in travel medicine, as they can provide up-to-date information on the specific risks and preventive measures for the destination you plan to visit.
When traveling to malaria-endemic areas, it is essential to take the necessary precautions to avoid mosquito bites. Mosquitoes that carry the malaria parasite are most active during the evening and nighttime hours, so it is advisable to wear long-sleeved shirts, long pants, and socks to cover exposed skin.
Additionally, applying insect repellent containing DEET (N, N-diethyl-meta-toluamide) or other recommended ingredients can provide further protection.
Another preventive measure is to sleep under a mosquito net treated with insecticide.
This creates a physical barrier between you and the mosquitoes while also killing any insects that come into contact with the net. It is important to ensure that the net is properly tucked in and does not have any holes or gaps that mosquitoes can enter through.
Furthermore, it is crucial to be aware of the symptoms of malaria, as early diagnosis and treatment can significantly improve outcomes. Symptoms may include fever, chills, headache, muscle aches, fatigue, nausea, and vomiting.
If you experience any of these symptoms during or after your trip to a malaria-endemic area, seek medical attention immediately and inform the healthcare provider about your travel history.
Remember, prevention is key when it comes to malaria. By taking the necessary precautions and following the advice of healthcare professionals, you can significantly reduce the risk of contracting this potentially life-threatening disease while traveling to malaria-endemic areas.
Weak Immune System
Individuals with weakened immune systems, such as young children, pregnant women, and people living with HIV/AIDS, are more vulnerable to severe malaria. Their bodies have difficulty fighting off the parasites, leading to more severe symptoms and complications.
Prevention tip: Pregnant women should receive regular antenatal care to prevent and manage malaria during pregnancy. Immunization and antiretroviral therapy can help individuals with HIV/AIDS strengthen their immune systems and reduce the risk of malaria.
In addition to young children, pregnant women, and people living with HIV/AIDS, other groups of individuals may have weakened immune systems and are at a higher risk of severe malaria. These include the elderly, individuals undergoing chemotherapy or radiation therapy for cancer, and those with certain autoimmune diseases.
For the elderly, the natural aging process weakens the immune system, making them more susceptible to infections like malaria. Healthcare providers must educate this population about the importance of preventive measures, such as using insecticide-treated bed nets and taking antimalarial medications.
Individuals undergoing chemotherapy or radiation therapy for cancer are also at an increased risk of severe malaria due to the immunosuppressive effects of these treatments. It is essential for healthcare professionals to closely monitor these patients and take proactive measures to prevent malaria infection, such as prescribing prophylactic antimalarial medications and recommending strict adherence to mosquito bite prevention strategies.
Furthermore, individuals with autoimmune diseases, such as lupus or rheumatoid arthritis, often take medications that suppress their immune system to manage their condition. While these medications are necessary for controlling their autoimmune disease, they can also increase their vulnerability to severe malaria.
Therefore, individuals with autoimmune diseases must work closely with their healthcare providers to develop a comprehensive plan that includes both disease management and malaria prevention strategies.
In conclusion, individuals with weakened immune systems, including young children, pregnant women, people living with HIV/AIDS, the elderly, those undergoing cancer treatment, and individuals with autoimmune diseases, are at a higher risk of severe malaria.
Healthcare providers need to recognize these vulnerable populations and provide them with targeted interventions to prevent and manage malaria effectively. In addition to the lack of access to healthcare services, several other factors contribute to the persistence of malaria in certain regions.
One such factor is the lack of awareness and education about the disease. Many people in malaria-endemic areas may not fully understand the causes, symptoms, and prevention methods associated with the disease.
Furthermore, the lack of proper infrastructure and resources in these areas also plays a significant role in hindering the efforts to control and eliminate malaria.
Inadequate sanitation facilities, limited access to clean water, and poor housing conditions create an environment that is conducive to the breeding of mosquitoes, the primary vector for malaria transmission.
Moreover, socio-economic factors such as poverty and inequality further exacerbate the problem. Individuals living in poverty often lack the means to afford preventive measures such as insecticide-treated bed nets or to seek timely medical care when symptoms arise. This perpetuates the cycle of transmission and makes it difficult to break the chain of infection.
Addressing these underlying factors requires a multi-faceted approach. Governments and international organizations need to invest in improving healthcare infrastructure, particularly in remote and resource-limited areas.
This includes increasing the availability of diagnostic tools and effective antimalarial medications, as well as training healthcare workers to diagnose and treat malaria.
Additionally, there is a need for comprehensive awareness and education campaigns that target both the general population and healthcare professionals. These campaigns should focus on raising awareness about the importance of early diagnosis, prompt treatment, and preventive measures such as the use of bed nets and insect repellents.
Furthermore, efforts to address the socio-economic factors that contribute to the persistence of malaria should be prioritized. This includes implementing poverty alleviation programs, improving access to education and employment opportunities, and addressing issues of inequality and social exclusion.
By addressing these underlying factors, we can hope to make significant progress in the fight against malaria. However, it is important to recognize that this is a complex and long-term endeavor that requires sustained commitment and collaboration from governments, international organizations, and communities affected by the disease.
Research and Development
Continued research and development of new antimalarial drugs is crucial in the fight against drug-resistant strains of malaria. As the malaria parasites continue to evolve and develop resistance to commonly used antimalarial drugs, it is essential to stay one step ahead by discovering and producing new drugs that can effectively treat the infection.
Researchers are constantly working to identify new compounds and molecules that have antimalarial properties. These compounds undergo rigorous testing in laboratories and animal models to determine their efficacy and safety. Promising candidates then move on to clinical trials, where they are tested in humans to assess their effectiveness in treating malaria.
Additionally, researchers are also exploring alternative treatment methods, such as gene editing and immunotherapy, to target and eradicate the malaria parasites. Gene editing techniques like CRISPR-Cas9 have shown promise in disrupting the genes responsible for drug resistance in the parasites, making them susceptible to existing antimalarial drugs.
Furthermore, the development of vaccines against malaria is another area of active research. Vaccines work by stimulating the immune system to recognize and attack the malaria parasites, preventing infection or reducing the severity of symptoms.
The most advanced malaria vaccine to date is RTS,S, which has shown partial effectiveness in clinical trials and is currently being piloted in selected areas of Africa.
In conclusion, research and development efforts are essential in the fight against malaria. By continuously discovering and producing new antimalarial drugs, exploring alternative treatment methods, and developing effective vaccines, we can overcome the challenges posed by drug resistance and ultimately work towards the eradication of malaria.
Climate change is a pressing issue that has far-reaching consequences for various aspects of our lives, including public health. The impact of climate change on the spread and intensity of malaria cannot be ignored.
As temperatures continue to rise and rainfall patterns become more unpredictable, the conditions for mosquito breeding become increasingly favorable, leading to an expansion in the geographical range of malaria transmission.
One of the key factors contributing to the spread of malaria is the increase in the number of mosquitoes. Mosquitoes thrive in warm and humid environments, and as temperatures rise, their population grows.
Additionally, altered rainfall patterns result in stagnant water, which serves as breeding grounds for mosquitoes. These climate changes create ideal conditions for the proliferation of malaria-carrying mosquitoes, posing a significant threat to public health.
To combat the impact of climate change on malaria transmission, it is crucial to adopt sustainable practices and policies that mitigate its effects.
This involves reducing greenhouse gas emissions, promoting renewable energy sources, and implementing measures to adapt to changing climatic conditions. By addressing the root causes of climate change, we can minimize its impact on the spread of malaria.
Furthermore, targeted mosquito control measures should be implemented in high-risk areas to reduce the mosquito population and prevent the transmission of malaria.
These measures may include the use of insecticides, mosquito nets, and the elimination of mosquito breeding sites. It is also essential to educate communities about the importance of personal protection measures, such as wearing protective clothing and using insect repellents.
However, it is not enough to focus solely on mosquito control. Environmental conservation plays a crucial role in minimizing mosquito breeding sites and reducing the risk of malaria transmission.
By preserving natural habitats, we can maintain a balance in ecosystems and prevent the proliferation of mosquitoes. This involves protecting wetlands, forests, and other natural areas that serve as mosquito breeding grounds.
In conclusion, climate change has a significant impact on the spread and intensity of malaria. To effectively combat this public health challenge, it is imperative to address the root causes of climate change through sustainable practices and policies.
Simultaneously, targeted mosquito control measures and environmental conservation efforts should be implemented to minimize mosquito breeding sites and reduce the risk of malaria transmission.
By adopting a comprehensive approach, we can work towards mitigating the impact of climate change on malaria and safeguarding public health. Community engagement plays a crucial role in the success of malaria prevention and control efforts.
When communities are actively involved and informed about the transmission, prevention, and treatment of malaria, they become empowered to take ownership of control initiatives. However, the lack of community engagement can pose significant challenges.
One of the main reasons for the lack of community engagement is the limited awareness and misconceptions surrounding malaria. In many affected areas, people may not fully understand how the disease is transmitted or the importance of preventive measures.
This lack of knowledge can lead to hesitancy in adopting preventive measures and hinder the effectiveness of interventions.
To address this issue, it is crucial to conduct community education programs that specifically target malaria prevention and control. These programs should involve local leaders, community members, and health professionals who can provide accurate information and dispel any misconceptions.
By educating the community about the transmission dynamics, symptoms, and available treatment options, individuals will be better equipped to protect themselves and their families.
Furthermore, community engagement should go beyond mere information dissemination. It is essential to empower communities to actively participate in malaria control initiatives. This can be achieved by involving them in decision-making processes, such as the selection of prevention strategies, distribution of bed nets, and implementation of indoor residual spraying.
Engaging community leaders and influential individuals is also crucial. These leaders can play a significant role in mobilizing their communities, creating awareness, and promoting preventive measures. By harnessing their influence and support, the message of malaria prevention can reach a wider audience and have a more significant impact.
In addition to education and empowerment, it is essential to establish channels of communication between the community and healthcare providers.
This can help address any concerns or misconceptions that individuals may have and facilitate the timely reporting and management of malaria cases.
Regular feedback sessions and community meetings can provide a platform for dialogue and collaboration between healthcare providers and community members. Overall, community engagement is a vital component of successful malaria prevention and control efforts.
By raising awareness, dispelling misconceptions, and empowering communities, we can ensure that everyone is actively involved in the fight against malaria. Together, we can make significant progress in reducing the burden of this deadly disease and improving the health and well-being of affected communities.
Poverty and Socioeconomic Factors
Poverty and socioeconomic factors contribute to the persistence of malaria. Limited access to healthcare, inadequate housing, and lack of resources for preventive measures increase the vulnerability of communities to malaria infection.
Poverty is a significant barrier to healthcare access, as individuals living in poverty often cannot afford medical treatment or preventive measures such as mosquito nets or insecticides.
In addition, inadequate housing conditions, such as overcrowding and lack of proper sanitation facilities, create breeding grounds for mosquitoes, increasing the risk of malaria transmission.
Furthermore, poverty often goes hand in hand with limited education and awareness about malaria prevention and control. Without proper education, individuals may not understand the importance of using mosquito nets, seeking early treatment, or eliminating mosquito breeding sites.
Lack of knowledge about the disease and its transmission can perpetuate the cycle of malaria in impoverished communities. Addressing poverty and socioeconomic factors is crucial in the fight against malaria.
Poverty alleviation programs can help improve the economic conditions of communities, providing them with the means to afford healthcare services and preventive measures. These programs can include initiatives such as microfinance, vocational training, and job creation, empowering individuals to lift themselves out of poverty.
Improving access to education is another vital aspect of tackling malaria. By investing in education, communities can gain knowledge about malaria prevention and control, empowering individuals to take proactive measures against the disease.
Education can also help raise awareness about the importance of seeking early treatment and adhering to prescribed antimalarial medications. Targeted interventions in high-risk populations are also necessary to reduce the burden of malaria.
These interventions can include community-based campaigns that distribute mosquito nets, insecticides, and antimalarial medications to vulnerable populations. Additionally, health education programs can be implemented to raise awareness about malaria prevention and control strategies.
Insufficient Vector Control
Effective vector control measures, such as indoor residual spraying and insecticide-treated bed nets, are crucial in reducing the transmission of malaria. Insufficient implementation and coverage of these interventions can lead to increased mosquito populations and malaria cases.
Prevention tip: Scale up vector control interventions, ensuring universal access to insecticide-treated bed nets and indoor residual spraying. Monitor insecticide resistance and adapt control strategies accordingly.
Vector control plays a vital role in preventing the spread of vector-borne diseases like malaria. Mosquitoes are the primary vectors of malaria, and controlling their populations is crucial in reducing the transmission of the disease.
Indoor residual spraying involves the application of insecticides to the interior walls of houses, targeting mosquitoes that come into contact with the treated surfaces. This method is highly effective in killing mosquitoes and reducing their populations.
Insecticide-treated bed nets are another essential tool in vector control. These nets are treated with insecticides that repel and kill mosquitoes upon contact.
When properly used, they create a physical barrier between individuals and mosquitoes, preventing bites and reducing the risk of malaria transmission. Universal access to insecticide-treated bed nets is essential to ensure that everyone at risk of malaria can protect themselves.
However, despite the effectiveness of these interventions, their implementation and coverage are often insufficient in many malaria-endemic regions. Limited resources, logistical challenges, and lack of awareness can hinder the widespread adoption of vector control measures. As a result, mosquito populations can thrive, leading to an increase in malaria cases.
To address this issue, it is crucial to scale up vector control interventions. Governments, international organizations, and local communities should prioritize the distribution and use of insecticide-treated bed nets and indoor residual spraying.
This includes ensuring that these interventions reach remote and underserved areas where malaria transmission is often high. Additionally, monitoring insecticide resistance is essential to ensure the continued effectiveness of these control strategies.
Regular surveillance can help identify emerging resistance and guide the selection of appropriate insecticides. Adapting control strategies based on the monitoring results is crucial to stay ahead of mosquito populations and prevent the spread of malaria.
This may involve changing the type or combination of insecticides used, implementing alternative vector control methods, or adjusting the timing and frequency of interventions. Flexibility and innovation in vector control approaches are key to effectively combat malaria and reduce its burden on affected communities.
Can pregnant women travel to malaria-endemic areas?
Pregnant women are at an increased risk of developing severe malaria and experiencing adverse outcomes if infected. Therefore, it is generally recommended that pregnant women avoid traveling to malaria-endemic areas.
If travel is unavoidable, it is essential for pregnant women to take extra precautions, such as using mosquito nets, wearing protective clothing, and taking antimalarial medications prescribed by a healthcare professional.
Are children more susceptible to malaria?
Yes, children, especially those under the age of five, are more susceptible to malaria infection and its severe complications. Their immune systems are not fully developed, making them more vulnerable to the parasites.
It is crucial to take extra precautions when traveling with children to malaria-endemic areas, such as ensuring they sleep under insecticide-treated bed nets and using child-friendly insect repellents.
Can malaria be diagnosed accurately?
Yes, malaria can be diagnosed accurately through laboratory tests. The most common method is the microscopic examination of blood samples to detect the presence of malaria parasites.
Rapid diagnostic tests (RDTs) are also available, which provide quick results and are particularly useful in resource-limited settings where microscopy may not be readily available.
Can mosquitoes become resistant to insecticides?
Yes, mosquitoes can develop resistance to insecticides over time. This is a significant concern in malaria control efforts as it can reduce the effectiveness of insecticide-treated bed nets and indoor residual spraying.
To combat this, ongoing research is focused on developing new insecticides and implementing strategies to manage and monitor insecticide resistance.
Is malaria a preventable disease?
Yes, malaria is a preventable disease. Through a combination of vector control measures, such as using insecticide-treated bed nets and indoor residual spraying, and prompt diagnosis and treatment of infected individuals, malaria transmission can be significantly reduced.
Additionally, efforts to develop an effective malaria vaccine are underway, which could further contribute to the prevention of the disease.
In conclusion,
poverty and socioeconomic factors play a significant role in the persistence of malaria. To effectively combat the disease, it is crucial to address these underlying issues through poverty alleviation programs, improved access to education, and economic opportunities.
By targeting interventions in high-risk populations and promoting awareness about malaria prevention, we can make significant strides in reducing the burden of malaria and improving the health and well-being of communities affected by this devastating disease.
Health
Understanding the Risk Factors for Developing Preeclampsia
Understanding the Risk Factors for Developing Preeclampsia
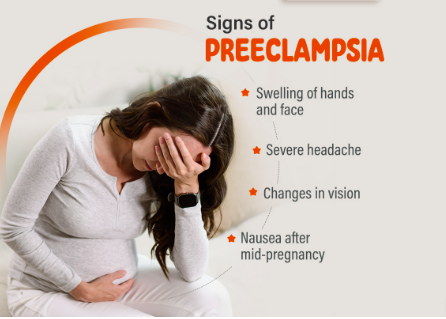
Preeclampsia is a serious pregnancy complication characterized by high blood pressure and potential damage to organs such as the liver and kidneys.
It usually occurs after the 20th week of pregnancy and can have significant implications for both the mother and the baby.
Identifying the risk factors associated with preeclampsia is crucial for early intervention and management.
This article delves into the various risk factors, how they contribute to the development of preeclampsia and strategies for monitoring and prevention.
What Is Preeclampsia?
Preeclampsia is a condition that affects approximately 5-8% of pregnancies worldwide. It typically manifests with elevated blood pressure and proteinuria (excess protein in the urine).
If left untreated, it can lead to severe complications such as eclampsia, which involves seizures and can jeopardize both maternal and fetal health.
Risk Factors for Preeclampsia
Understanding the risk factors for preeclampsia can help in early diagnosis and management. Below are the primary risk factors associated with this condition:
1. Previous History of Preeclampsia
Women who have experienced preeclampsia in previous pregnancies are at a higher risk of developing the condition in subsequent pregnancies. The recurrence risk is approximately 20-30% if preeclampsia occurs in a previous pregnancy.
2. First Pregnancy
The risk of preeclampsia is higher in women who are pregnant for the first time. This is thought to be related to the body’s adjustment to the physiological changes associated with pregnancy.
3. Advanced Maternal Age
Women who are over the age of 35 are more likely to develop preeclampsia. The increased risk is associated with age-related changes in blood vessels and the body’s ability to manage pregnancy-related stress.
4. Multiple Gestations
Carrying more than one baby (e.g., twins or triplets) increases the risk of preeclampsia. The body’s increased demands and altered placental development contribute to this heightened risk.
5. Obesity
Obesity is a significant risk factor for preeclampsia. Excess body weight can lead to increased blood pressure and insulin resistance, both of which are associated with a higher likelihood of developing preeclampsia.
6. Chronic Hypertension
Women with pre-existing high blood pressure are at a greater risk of developing preeclampsia. Chronic hypertension can exacerbate the blood pressure problems associated with preeclampsia.
7. Diabetes
Both type 1 and type 2 diabetes are associated with an increased risk of preeclampsia. Diabetes can affect blood vessel function and increase the likelihood of high blood pressure during pregnancy.
8. Kidney Disease
Pre-existing kidney conditions can elevate the risk of preeclampsia. The kidneys play a crucial role in managing blood pressure and fluid balance, and any pre-existing conditions can compromise their function.
9. Autoimmune Disorders
Certain autoimmune disorders, such as lupus and rheumatoid arthritis, can increase the risk of developing preeclampsia. These conditions can affect the body’s immune response and vascular health.
10. Family History
A family history of preeclampsia can indicate a genetic predisposition to the condition. Women with a family history are at an increased risk compared to those without such a history.
11. Poor Nutrition
Inadequate nutrition, particularly a lack of essential vitamins and minerals such as calcium and magnesium, can contribute to the development of preeclampsia. Proper prenatal care and nutrition are crucial for minimizing risk.
12. Infections
Certain infections during pregnancy, such as urinary tract infections, can be associated with an increased risk of preeclampsia. Infections can exacerbate the inflammatory processes involved in preeclampsia.
13. High Stress Levels
Chronic stress and poor mental health can impact overall well-being and contribute to conditions like preeclampsia. Managing stress through healthy lifestyle choices and support systems is important.
Monitoring and Prevention Strategies
Early monitoring and preventive measures can help manage the risk factors associated with preeclampsia:
- Regular Prenatal Visits: Frequent check-ups with a healthcare provider can help monitor blood pressure and other indicators of preeclampsia.
- Healthy Lifestyle Choices: Maintaining a balanced diet, engaging in regular physical activity, and managing weight can reduce the risk.
- Medication: In some cases, medications such as aspirin may be recommended to lower the risk of preeclampsia, especially for women with a high risk.
- Stress Management: Techniques such as mindfulness, relaxation exercises, and counseling can help manage stress and support overall health.
- Education and Awareness: Understanding the symptoms and risk factors of preeclampsia can help in early detection and timely intervention.
Conclusion
Preeclampsia is a complex condition with multiple risk factors. By recognizing these factors and taking proactive steps, expectant mothers can work with their healthcare providers to manage their risk and promote a healthier pregnancy.
Regular prenatal care, lifestyle modifications, and stress management are key to minimizing the impact of preeclampsia and ensuring the best possible outcomes for both mother and baby.
FAQs
1. What are the early signs of preeclampsia?
Early signs of preeclampsia include high blood pressure, proteinuria, swelling of the hands and feet, sudden weight gain, and severe headaches. It’s important to report any unusual symptoms to your healthcare provider promptly.
2. Can preeclampsia be prevented?
While not all cases of preeclampsia can be prevented, maintaining a healthy lifestyle, attending regular prenatal visits, and following your healthcare provider’s recommendations can help reduce the risk.
3. How is preeclampsia diagnosed?
Preeclampsia is diagnosed through routine prenatal screenings that monitor blood pressure and urine protein levels. If preeclampsia is suspected, additional tests may be conducted to assess kidney function and other health indicators.
4. What are the treatment options for preeclampsia?
Treatment options for preeclampsia depend on the severity of the condition. They may include medications to manage blood pressure, bed rest, and in severe cases, early delivery of the baby to protect both the mother and child.
5. Can preeclampsia affect future pregnancies?
Having preeclampsia in one pregnancy can increase the risk of developing it in future pregnancies. However, many women go on to have healthy pregnancies by managing risk factors and following their healthcare provider’s advice.
References:
Health
Top 5 Immunity-Boosting Fruits to Include in Your Diet

Top 5 Immunity-Boosting Fruits to Include in Your Diet
In our quest for better health, the immune system often takes center stage. One of the simplest and most effective ways to support this vital system is through a nutritious diet.
Fruits, rich in essential vitamins, minerals, and antioxidants, can play a significant role in strengthening your immune system.
In this article, we’ll explore the best fruits for boosting immunity, backed by scientific research, and provide practical tips for incorporating them into your daily routine.
Why Immune Health Matters
The immune system is our body’s defense mechanism against harmful pathogens, including bacteria, viruses, and toxins.
A robust immune system can help fend off illnesses and infections, and a balanced diet is crucial for maintaining its optimal function.
Fruits, in particular, offer a wealth of nutrients that can enhance immune response, improve overall health, and even prevent chronic diseases.
1. Citrus Fruits: Vitamin C Powerhouses
Oranges
Oranges are synonymous with vitamin C, a crucial nutrient for immune health. Vitamin C supports the production and function of white blood cells, which are essential for fighting infections.
Just one medium-sized orange provides about 70 mg of vitamin C, meeting the daily recommended intake for most adults.
Grapefruits
Grapefruits, another excellent source of vitamin C, also contain antioxidants like lycopene, which have been linked to reduced inflammation and improved immune function.
Enjoying half a grapefruit a day can contribute significantly to your vitamin C needs.
Lemons
Lemons are versatile fruits that not only boost your vitamin C intake but also support detoxification.
Adding lemon juice to water or dishes can enhance your immune system while providing a refreshing flavor.
2. Berries: Antioxidant-Rich Superfoods
Blueberries
Blueberries are packed with antioxidants, particularly flavonoids, which help combat oxidative stress and inflammation.
These antioxidants can enhance immune function and protect against chronic diseases. A cup of fresh blueberries is a delicious way to boost your immunity.
Strawberries
Strawberries are another berry with a high vitamin C content, along with various antioxidants that contribute to overall health.
A handful of strawberries can provide a significant portion of your daily vitamin C requirement.
Raspberries
Raspberries are rich in vitamins C and E, as well as fiber and antioxidants.
These nutrients work together to support immune health and maintain digestive well-being.
Incorporate raspberries into smoothies or salads for a tasty immune boost.
4. Papaya
Papaya is an excellent source of vitamin C, vitamin A, and digestive enzymes such as papain. These nutrients contribute to a stronger immune system by supporting cellular repair and reducing inflammation.
5. Pomegranate
Pomegranates are rich in antioxidants and vitamin C, which help combat oxidative stress and boost immune function. The anti-inflammatory properties of pomegranates also support overall health and wellness.
Incorporating these fruits into your daily diet can provide essential nutrients that support immune health and help protect your body against illnesses.
Frequently Asked Questions
1. How does vitamin C boost the immune system?
Vitamin C enhances the production of white blood cells, which are crucial for combating infections and illnesses. It also acts as an antioxidant, protecting cells from damage caused by free radicals.
2. Can berries help reduce inflammation?
Yes, berries are rich in antioxidants and vitamins that help reduce inflammation and oxidative stress, which can support overall immune function.
3. What are the benefits of kiwi for immune health?
Kiwi provide a high amount of vitamin C, which supports the immune system by increasing white blood cell production. It also contains vitamin K and folate, which are essential for maintaining overall health.
4. How does papaya contribute to immune health?
Papaya is high in vitamin C and vitamin A, which help strengthen the immune system. Additionally, the enzyme papain in papaya aids in digestion and reduces inflammation.
5. What makes pomegranates beneficial for immunity?
Pomegranates are rich in antioxidants and vitamin C, which help fight oxidative stress and inflammation, thereby supporting the immune system and overall health.
References:
Healthline – Best Fruits for Boosting Immunity
Health
Effective Medications to Lower Cholesterol: A Comprehensive Guide

Effective Medications to Lower Cholesterol: A Comprehensive Guide
High cholesterol is a common health issue that can significantly increase the risk of heart disease, stroke, and other serious health conditions. Fortunately, various medications are available to help manage and lower cholesterol levels.
In this guide, we’ll explore the most effective medications for lowering cholesterol, their mechanisms of action, potential side effects, and other crucial information to help you make informed decisions about your health.
Understanding Cholesterol and Its Impact on Health
Cholesterol is a fatty substance found in your blood. Your body needs cholesterol to build healthy cells, but having high levels of cholesterol can increase your risk of heart disease.
Cholesterol travels through your bloodstream in two main types of lipoproteins:
low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
- LDL Cholesterol: Often referred to as “bad” cholesterol, LDL can build up in the walls of your arteries, leading to atherosclerosis, which can restrict blood flow and increase the risk of heart attacks and strokes.
- HDL Cholesterol: Known as “good” cholesterol, HDL helps remove LDL cholesterol from your arteries, reducing the risk of cardiovascular problems.
Why Medication May Be Necessary
Even with a healthy diet and regular exercise, some individuals may still struggle to manage their cholesterol levels.
This is where cholesterol-lowering medications come into play. These medications work in various ways to help lower LDL cholesterol and, in some cases, raise HDL cholesterol.
Types of Cholesterol-Lowering Medications
1. Statins
Statins are the most commonly prescribed medications for lowering LDL cholesterol.
They work by blocking a substance your body needs to make cholesterol, thus reducing the amount of LDL cholesterol in your bloodstream.
- Examples: Atorvastatin (Lipitor), Simvastatin (Zocor), Rosuvastatin (Crestor)
- Mechanism of Action: Statins inhibit the enzyme HMG-CoA reductase, which is involved in cholesterol production in the liver.
- Common Side Effects: Muscle pain, digestive problems, increased liver enzymes
- Benefits: Statins are highly effective in reducing LDL cholesterol levels and have been shown to lower the risk of heart attacks and strokes.
2. Bile Acid Sequestrants
Bile acid sequestrants work by binding to bile acids in the intestine, preventing them from being reabsorbed. This process forces the liver to use cholesterol to produce more bile acids, thus lowering LDL cholesterol levels.
- Examples: Cholestyramine (Prevalite), Colestipol (Colestid), Colesevelam (Welchol)
- Mechanism of Action: These drugs bind bile acids in the intestines, reducing cholesterol absorption.
- Common Side Effects: Constipation, bloating, nausea
- Benefits: Effective at lowering LDL cholesterol and can be used in conjunction with statins for enhanced results.
3. Niacin
Niacin (also known as vitamin B3) helps lower LDL cholesterol and raise HDL cholesterol levels.
It works by decreasing the liver’s production of LDL cholesterol and increasing HDL cholesterol.
- Examples: Niacor, Niaspan
- Mechanism of Action: Niacin reduces the production of LDL cholesterol and increases HDL cholesterol.
- Common Side Effects: Flushing, itching, liver damage (with high doses)
- Benefits: Effective in raising HDL cholesterol and lowering LDL cholesterol.
4. Fibric Acids
Fabric acids, or fibrates, are primarily used to lower triglyceride levels and can also help increase HDL cholesterol levels.
They work by activating a protein that helps break down triglycerides in the blood.
- Examples: Fenofibrate (Tricor), Gemfibrozil (Lopid)
- Mechanism of Action: They activate peroxisome proliferator-activated receptors (PPARs), which help in the breakdown of triglycerides.
- Common Side Effects: Muscle pain, liver abnormalities, gastrointestinal issues
- Benefits: Particularly useful for individuals with high triglyceride levels.
5. PCSK9 Inhibitors
PCSK9 inhibitors are a newer class of cholesterol-lowering medications that help the liver remove LDL cholesterol from the bloodstream more effectively.
- Examples: Alirocumab (Praluent), Evolocumab (Repatha)
- Mechanism of Action: These drugs inhibit the PCSK9 protein, which normally reduces the liver’s ability to remove LDL cholesterol from the blood.
- Common Side Effects: Injection site reactions, flu-like symptoms
- Benefits: Very effective at lowering LDL cholesterol, especially in individuals who cannot tolerate statins.
6. Cholesterol Absorption Inhibitors
Cholesterol absorption inhibitors work by blocking the absorption of cholesterol from the diet, which reduces the amount of cholesterol that enters your bloodstream.
- Examples: Ezetimibe (Zetia)
- Mechanism of Action: They inhibit the absorption of cholesterol in the small intestine.
- Common Side Effects: Diarrhea, stomach pain, muscle pain
- Benefits: Can be used alone or in combination with statins to lower LDL cholesterol.
Choosing the Right Medication
The choice of medication depends on various factors, including your overall health, the specific cholesterol issue you have, and how well you tolerate certain medications.
Your healthcare provider will help you determine the most appropriate medication based on your individual needs and medical history.
Lifestyle Modifications to Complement Medication
While medications are effective in managing cholesterol levels, they work best when combined with lifestyle changes.
Consider incorporating the following into your routine:
- Healthy Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins while avoiding saturated fats and trans fats.
- Regular Exercise: Engage in at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity per week.
- Weight Management: Achieve and maintain a healthy weight to help control cholesterol levels.
- Avoid Smoking and Limit Alcohol: Both smoking and excessive alcohol intake can negatively impact cholesterol levels.
Monitoring and Follow-Up
Regular follow-up with your healthcare provider is crucial to monitor your cholesterol levels and assess the effectiveness of your medication. Your doctor may adjust your treatment plan based on your progress and any side effects you experience.
Final Thoughts
Managing cholesterol is a critical aspect of maintaining cardiovascular health.
With a variety of effective medications available, it’s possible to lower LDL cholesterol levels and reduce the risk of heart disease and other complications.
However, medication alone is not a cure-all; combining it with lifestyle changes is essential for optimal results.
Always consult your healthcare provider for personalized advice and treatment plans tailored to your specific needs.
Frequently Asked Questions (FAQs)
1. What is the primary goal of cholesterol-lowering medications?
Cholesterol-lowering medications primarily aim to reduce LDL cholesterol levels in the blood, thereby decreasing the risk of cardiovascular diseases such as heart attacks and strokes.
2. Are there any natural alternatives to cholesterol-lowering medications?
Yes, some natural alternatives include dietary changes (e.g., increased intake of soluble fiber and omega-3 fatty acids), regular exercise, and weight management. However, these should be used in conjunction with, not as a replacement for, prescribed medications.
3. How long does it take for cholesterol-lowering medications to show results?
The effects of cholesterol-lowering medications can usually be observed within a few weeks, but it may take several months to see significant changes in cholesterol levels and overall cardiovascular risk.
4. Can cholesterol-lowering medications cause side effects?
Yes, some common side effects include muscle pain, digestive issues, and liver enzyme changes. It’s important to report any side effects to your healthcare provider for proper management.
5. Can I stop taking my cholesterol medication if my levels improve?
It’s important to consult your healthcare provider before making any changes to your medication regimen. Discontinuing medication without medical advice can lead to a rebound in cholesterol levels and an increased risk of heart disease.
References
Cholesterol-lowering Medications
-

 Trending Stories1 year ago
Trending Stories1 year agoCDC: 1 in 4 Americans Still COVID-Free by End of 2022
-

 Health5 years ago
Health5 years agoMeghan Trainor Shares Motivational New Song ‘Blink’
-

 Health2 years ago
Health2 years agoHow Long Does Monkey Pox Last Before It Surfaces in the Body?
-

 Health2 years ago
Health2 years agoWhat Causes Swollen Body? Understanding Edema and its Triggers
-

 Health3 years ago
Health3 years agoNutrition and the Importance of a Fitness Program – 3 Things to Know
-

 Health3 years ago
Health3 years ago5 Weird Reasons Why Pimples Disappear After Marriage
-

 Health3 months ago
Health3 months agoHow Do Pawpaw Seeds Support Cardiovascular Health?
-

 Health2 years ago
Health2 years agoHealth Benefits Of Pawpaw Seed? 7 Things To Know





