Health
Prevention and Control of Measles in Children: The Most Common Causes and Solutions

Last Updated on May 18, 2023 by Nurse Vicky
Prevention and Control of Measles in Children: The Most Common Causes and Solutions
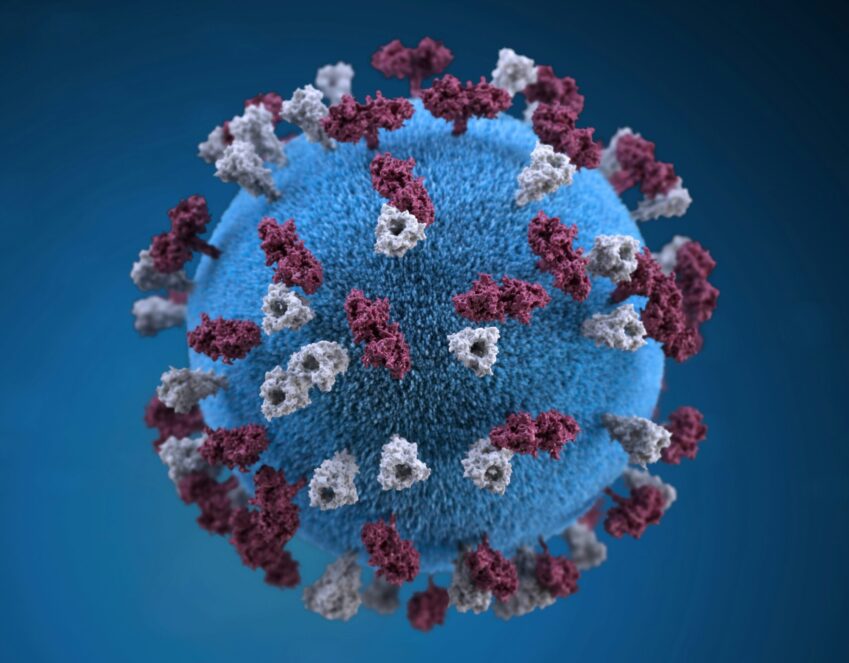
Measles is a highly contagious viral infection that primarily affects children. It spreads rapidly and can lead to serious complications if left untreated. In this comprehensive guide, we will delve into the most common causes of measles in children and explore effective prevention and control measures.
By understanding the underlying factors and implementing appropriate strategies, we can safeguard the health and well-being of our children. Understanding Measles Measles, also known as rubeola, is caused by the measles virus (MeV).
It is transmitted through respiratory droplets when an infected person coughs or sneezes. The virus can survive in the air or on surfaces for up to two hours, making it highly contagious. Once contracted, it takes about 10-14 days for symptoms to appear.
Symptoms of Measles The initial symptoms of measles often resemble those of a common cold, including fever, cough, runny nose, and red, watery eyes. Within a few days, small white spots known as Koplik’s spots may appear inside the mouth. A rash then develops, starting on the face and gradually spreading to the rest of the body.
Complications Associated with Measles While most cases of measles resolve without complications, it can lead to severe health issues, especially in young children. Some of the potential complications include ear infections, pneumonia, encephalitis (brain inflammation), and even death. Those with weakened immune systems are particularly vulnerable.
Causes of Measles Measles outbreaks often occur due to several contributing factors. One of the primary causes is a lack of vaccination or incomplete immunization. When a significant portion of the population is unvaccinated, the virus can easily spread. Additionally, international travel and migration can introduce the virus to susceptible populations.
Vaccine Hesitancy and Misinformation Vaccine hesitancy, driven by misinformation and misconceptions, plays a significant role in the persistence of measles cases.
Some individuals harbor concerns about vaccine safety, despite extensive research and evidence supporting the effectiveness and safety of measles vaccines. Addressing vaccine hesitancy is crucial to prevent future outbreaks.
Importance of Herd Immunity Herd immunity refers to a situation where a significant proportion of the population is immune to a particular disease, making it difficult for the virus to spread.
Achieving high vaccination rates is essential to establish and maintain herd immunity against measles. By protecting ourselves, we also protect those who are unable to receive vaccines due to medical reasons.
Prevention and Control Measures The most effective way to prevent measles is through vaccination. The measles-mumps-rubella (MMR) vaccine provides long-lasting immunity against the virus. It is administered in two doses, with the first dose given at around 12-15 months of age and the second dose between 4-6 years of age.
Immunization Campaigns and Outreach Programs To enhance vaccination rates, governments, and healthcare organizations conduct immunization campaigns and outreach programs.
These initiatives aim to increase awareness about the importance of vaccination, address concerns, and provide easy access to vaccines. Engaging communities and educating parents and caregivers are crucial components of such programs.
Public Health Surveillance and Early Detection Effective surveillance systems play a vital role in identifying and containing measles outbreaks. Rapid detection of cases allows for timely intervention, such as isolating infected individuals and administering post-exposure prophylaxis. Early detection minimizes the risk of transmission and helps control the spread of the virus.
Health Education and Awareness Education and awareness initiatives are pivotal in preventing measles. Parents, caregivers, and healthcare professionals should be educated Educating Parents and Caregivers Parents and caregivers need accurate information about measles to make informed decisions regarding vaccination and preventive measures.
Health education campaigns should provide clear and concise information about the benefits and safety of vaccines, debunk common myths, and emphasize the importance of timely immunization.
Strengthening Healthcare Systems A robust healthcare system is essential for effective measles prevention and control. It includes adequate vaccine supply, trained healthcare professionals, and efficient immunization programs. Governments should invest in strengthening healthcare infrastructure to ensure access to vaccines and quality healthcare services.
Strategies for Measles Control
Enhanced Vaccination Coverage Achieving and maintaining high vaccination coverage rates is key to measles control. National immunization programs should prioritize increasing access to vaccines, especially in underserved areas. Efforts should be made to reach marginalized populations and address barriers to vaccination, such as cost, transportation, and vaccine availability.
Rapid Response to Outbreaks Early detection and swift response to measles outbreaks are crucial. Health authorities should have well-defined outbreak response plans in place. These plans should include surveillance systems, outbreak investigation protocols, and mechanisms for delivering vaccines and providing supportive care to affected individuals.
Strengthening Routine Immunization Programs Routine immunization programs form the foundation of measles control. Governments and healthcare organizations must invest in strengthening these programs to ensure timely and complete immunization coverage for all eligible children. This includes improving vaccine delivery systems, monitoring coverage rates, and conducting regular immunization campaigns.
Frequently Asked Questions
Are measles vaccines safe?
Yes, measles vaccines are safe. Extensive research and monitoring have demonstrated their safety and effectiveness in preventing measles.
What are the side effects of the measles vaccine?
Common side effects of the measles vaccine include soreness at the injection site, low-grade fever, and a mild rash. Severe side effects are rare.
Can a person get measles even if they have been vaccinated?
While measles vaccines are highly effective, there is still a small chance of contracting the virus after vaccination. However, vaccinated individuals usually experience milder symptoms and complications.
At what age should children receive the measles vaccine?
The first dose of the measles vaccine is typically given at 12-15 months of age, with a second dose administered between 4-6 years of age.
How long does immunity from the measles vaccine last?
The measles vaccine provides long-lasting immunity. In most cases, immunity lasts throughout a person’s life.
Can adults get measles?
Yes, adults can get measles if they are not immune. It is important for adults to check their vaccination status and receive the vaccine if necessary.
Is measles contagious before symptoms appear?
Yes, measles can be contagious before symptoms appear. Infected individuals can spread the virus to others for several days before the rash develops.
Can measles be treated with antibiotics?
No, antibiotics are not effective against measles. Supportive care, such as rest, fluids, and fever-reducing medication, can help manage symptoms.
someone with measles?
If your child has been exposed to someone with measles, it is important to consult with a healthcare professional. They will assess your child’s vaccination status and provide guidance on the appropriate steps to take, which may include monitoring for symptoms or administering post-exposure prophylaxis.
Can measles be prevented through natural immunity?
Natural immunity to measles can be acquired by contracting and recovering from the virus. However, this approach is not recommended due to the risks of severe complications and the availability of safe and effective vaccines.
Are there any specific groups at higher risk of measles?
Yes, certain groups, such as infants, pregnant women, and individuals with weakened immune systems, are at higher risk of severe complications from measles. Vaccination and minimizing exposure to the virus are crucial for their protection.
Can measles be transmitted through breastfeeding?
Measles is not typically transmitted through breast milk. In fact, breastfeeding provides important antibodies that can help protect infants from the virus. However, if a breastfeeding mother has measles, it is important to take precautions to prevent direct contact with respiratory droplets.
Is there a cure for measles?
There is no specific cure for measles. Treatment involves managing symptoms and providing supportive care, such as rest, hydration, and fever-reducing medication.
Can measles be eradicated globally?
While the global eradication of measles is a challenging goal, it is achievable through coordinated efforts. Vaccination, surveillance, and public health measures have been successful in eliminating measles in several countries, and ongoing efforts aim to achieve worldwide eradication.
Can I travel if I have not been vaccinated against measles?
It is recommended to be vaccinated against measles before traveling, especially to areas with ongoing measles outbreaks. Vaccination helps protect both individuals and prevent the spread of the virus to susceptible populations.
Remember, if you have any specific concerns or questions about measles, it is always best to consult with a healthcare professional who can provide personalized advice based on your individual circumstances. Stay informed, prioritize vaccination, and take proactive steps to protect the health and well-being of children against measles.
Measles is a highly contagious viral disease, which requires strict hand hygiene. The best way to prevent it is by vaccination, but there are also other ways to prevent it. Those methods include isolation and antibiotics. The following tips can help you prevent measles.
Follow these guidelines to protect your child from contracting the illness. Also, follow these tips to avoid contracting the virus yourself.
Measles is a highly contagious viral illness
In most cases, the disease is mild and does not cause any complications, but in 1% of cases, it can lead to complications such as pneumonia or diarrhea. Subacute sclerosing panencephalitis (SSE), a potentially fatal condition, is a rare complication of measles. This occurs when the virus becomes persistent in the brain, and it is often fatal.
Measles vaccination is the best way to prevent it
The best way to protect yourself from measles is by getting vaccinated. The measles vaccine is a combination of the measles, mumps, and rubella vaccine (MMR).
The first dose of the MMR vaccine gives 93 percent protection, and the second booster dose improves this protection to 97 percent. Traveling outside the U.S. and other countries can increase your chances of contracting measles.
Isolation
The primary goal of measles isolation is to prevent the spread of the disease. The use of facemasks or other protective equipment for the nose and mouth should be followed for all contact investigations. In case of doubt, the use of a facemask or other protective equipment certified by the National Institute of Occupational Safety and Health (NIOSH) is recommended.
In the event of doubt, contact investigations should be guided by the Guideline for Isolation Precautions (Guideline for Isolation Precautions).
Antibiotics
This review assessed the effectiveness of antibiotics in the prevention and control of measles. It included seven controlled clinical trials. Five of these studies took place in Glasgow and London. One was conducted in India in the 1960s, and another was published in Bissau, Guinea-Bissau, West Africa.
These studies tended to use a different combination of antibiotics. The duration of treatment varied. Patients were given antibiotics for at least 10 days, and some complications were reported in approximately 1% of cases.
Avoiding measles during pregnancy
Measles is a highly contagious disease that can affect both adults and children. Symptoms of the disease include a high fever, runny nose, cough, and red, itchy eyes. Within one to two weeks, white spots appear inside the mouth.
Measles vaccination is not recommended during pregnancy. But you can still protect yourself and your baby. The following are a few precautions to take.
Vaccination
Vaccination for the prevention and control of measles is an important public health strategy, especially among young children. Measles was responsible for 2.6 million deaths globally before 1980 and is still the leading cause of death in children under five.
To achieve elimination, the Pan American Health Organization has set the goal of eliminating measles in the Americas by the year 2000. The disease can be eradicated by ensuring that the population receives two doses of the vaccine, one of each of the two main types.
While the vaccine is equally safe, it is usually incorporated with the rubella vaccine. Adding rubella to the measles vaccine increases its cost and allows for shared delivery costs.
Treatment
Measles symptoms in infants and young children have distinct characteristics. Compared to older children, infants do not develop a fever, runny nose, or Filatov-Koplik spots.
In children, measles rash is small and does not last for more than two days. Infants and young children may suffer from bacterial complications like pneumonia, otitis media, and intestinal upset.
Frequently Asked Questions
Are measles vaccines safe?
Yes, measles vaccines are safe. Extensive research and monitoring have demonstrated their safety and effectiveness in preventing measles.
What are the side effects of the measles vaccine?
Common side effects of the measles vaccine include soreness at the injection site, low-grade fever, and a mild rash. Severe side effects are rare.
Can a person get measles even if they have been vaccinated?
While measles vaccines are highly effective, there is still a small chance of contracting the virus after vaccination. However, vaccinated individuals usually experience milder symptoms and complications.
At what age should children receive the measles vaccine?
The first dose of the measles vaccine is typically given at 12-15 months of age, with a second dose administered between 4-6 years of age.
How long does immunity from the measles vaccine last?
The measles vaccine provides long-lasting immunity. In most cases, immunity lasts throughout a person’s life.
Can adults get measles?
Yes, adults can get measles if they are not immune. It is important for adults to check their vaccination status and receive the vaccine if necessary.
Is measles contagious before symptoms appear?
Yes, measles can be contagious before symptoms appear. Infected individuals can spread the virus to others for several days before the rash develops.
Can measles be treated with antibiotics?
No, antibiotics are not effective against measles. Supportive care, such as rest, fluids, and fever-reducing medication, can help manage symptoms.
someone with measles?
Can measles be prevented through natural immunity?
Natural immunity to measles can be acquired by contracting and recovering from the virus. However, this approach is not recommended due to the risks of severe complications and the availability of safe and effective vaccines.
Are there any specific groups at higher risk of measles?
Yes, certain groups, such as infants, pregnant women, and individuals with weakened immune systems, are at higher risk of severe complications from measles. Vaccination and minimizing exposure to the virus are crucial for their protection.
Can measles be transmitted through breastfeeding?
Measles is not typically transmitted through breast milk. In fact, breastfeeding provides important antibodies that can help protect infants from the virus. However, if a breastfeeding mother has measles, it is important to take precautions to prevent direct contact with respiratory droplets.
Is there a cure for measles?
There is no specific cure for measles. Treatment involves managing symptoms and providing supportive care, such as rest, hydration, and fever-reducing medication.
Can measles be eradicated globally?
While the global eradication of measles is a challenging goal, it is achievable through coordinated efforts. Vaccination, surveillance, and public health measures have been successful in eliminating measles in several countries, and ongoing efforts aim to achieve worldwide eradication.
Can I travel if I have not been vaccinated against measles?
It is recommended to be vaccinated against measles before traveling, especially to areas with ongoing measles outbreaks. Vaccination helps protect both individuals and prevent the spread of the virus to susceptible populations.
Remember, if you have any specific concerns or questions about measles, it is always best to consult with a healthcare professional who can provide personalized advice based on your individual circumstances. Stay informed, prioritize vaccination, and take proactive steps to protect the health and well-being of children against measles.
Measles is a highly contagious viral disease, which requires strict hand hygiene. The best way to prevent it is by vaccination, but there are also other ways to prevent it. Those methods include isolation and antibiotics. The following tips can help you prevent measles.
Follow these guidelines to protect your child from contracting the illness. Also, follow these tips to avoid contracting the virus yourself.
Conclusion
Prevention and control of measles in children require a multi-faceted approach that encompasses vaccination, education, and strengthening healthcare systems. Vaccination remains the most effective preventive measure, and efforts should be made to address vaccine hesitancy and ensure equitable access to vaccines.
Strong surveillance systems, rapid outbreak response, and robust routine immunization programs are vital components of measles control. By implementing these strategies, we can work towards eliminating measles and protecting the health of our children.
Health
Hair Gummies: A Trend Worth Your Time or Just Another Health Fad?

Hair Gummies: A Trend Worth Your Time or Just Another Health Fad?
In recent years, hair gummies have taken the health and beauty world by storm, boasting promises of luscious locks and a speedy route to hair health.
But with an array of products flooding the market, it’s essential to separate fact from fiction.
Are these colorful, chewy supplements a miracle solution for your hair troubles, or are they simply a trendy snack with little efficacy?
In this comprehensive article, we will explore the science behind hair gummies, their ingredients, potential benefits, and the questions surrounding their effectiveness.
Understanding Hair Health
The Basics of Hair Growth
To fully grasp the impact of hair gummies, it’s vital to understand how hair grows.
Each strand of hair goes through three main phases:
- Anagen Phase: This is the active growth phase, which can last several years. The length of this phase varies among individuals.
- Catagen Phase: A transitional phase lasting a few weeks, where hair growth slows, and the hair follicle shrinks.
- Telogen Phase: The resting phase, lasting a few months before the hair falls out, making way for new growth.
Hair health is influenced by a variety of factors, including genetics, hormones, diet, and overall health.
As such, a balanced approach to hair care, encompassing nutrition, proper hair care routines, and avoiding damaging practices, is essential.
Common Causes of Hair Issues
Hair loss or poor hair health can arise from numerous factors:
- Nutritional Deficiencies: A lack of essential vitamins and minerals can hinder hair growth.
- Hormonal Changes: Conditions like pregnancy, menopause, and thyroid disorders can significantly affect hair health.
- Stress: Chronic stress can trigger hair loss through a condition known as telogen effluvium.
- Medical Conditions: Certain diseases and medications can also contribute to hair loss.
What Are Hair Gummies?
Hair gummies are dietary supplements designed to promote hair health.
They are usually made with a combination of vitamins, minerals, and sometimes botanical extracts, often marketed as a convenient and tasty alternative to traditional vitamin pills.
Key Ingredients in Hair Gummies
While formulations vary, here are some common ingredients found in hair gummies:
- Biotin: A B-vitamin known for its role in hair and nail health. Biotin deficiencies can lead to brittle hair and hair loss.
- Vitamins A, C, and E: Antioxidants that help protect hair from oxidative stress, promoting a healthy scalp and hair growth.
- Folic Acid: Important for cell growth and regeneration, folic acid is believed to support healthy hair follicles.
- Zinc: Plays a role in hair tissue growth and repair, making it a crucial mineral for maintaining healthy hair.
- Collagen: An essential protein for skin elasticity that may also benefit hair strength and growth.
Do Hair Gummies Really Work?
The Science Behind Hair Gummies
While the ingredients in hair gummies are known to contribute to hair health, the question remains:
Do they work as effectively as claimed?
Here’s what the research suggests:
- Biotin: Studies have shown that biotin can improve hair thickness in those with deficiencies, but most people get sufficient biotin from their diet. Supplementing with biotin may not yield significant benefits for individuals who are not deficient.
- Vitamins and Minerals: Research indicates that vitamins A, C, D, E, and minerals like zinc and iron play a role in maintaining healthy hair. However, simply taking these vitamins in gummy form doesn’t guarantee results unless there’s a deficiency present.
- Collagen: Some studies suggest that collagen supplements can improve hair and skin health by providing amino acids essential for protein synthesis. However, more research is needed to establish direct benefits for hair growth.
User Experiences and Anecdotes
While anecdotal evidence often highlights positive experiences with hair gummies, it’s important to approach these testimonials with caution. Individual results may vary, and factors such as diet, overall health, and genetics play significant roles in hair health.
Potential Benefits of Hair Gummies
While not a miracle solution, hair gummies may offer certain benefits:
- Convenient Form: For those who struggle with swallowing pills, gummies provide a palatable alternative.
- Added Nutrients: If you have a deficiency in specific vitamins or minerals, hair gummies can supplement your diet effectively.
- Increased Awareness of Nutrition: Taking supplements can prompt individuals to pay more attention to their overall nutritional intake.
- Improved Hair Appearance: Users may notice shinier and healthier-looking hair due to the vitamins and antioxidants present in these products.
Are There Risks?
While hair gummies are generally safe, there are some considerations to keep in mind:
- Overconsumption: Gummies are often flavored and sweetened, which may lead to overconsumption and potential digestive issues.
- Sugar Content: Many gummies contain added sugars, which can contribute to other health problems if consumed excessively.
- Interactions with Other Supplements: If you’re taking other vitamins or supplements, it’s essential to ensure you’re not exceeding recommended doses, particularly for fat-soluble vitamins like A and E, which can accumulate in the body.
What Experts Say
Dermatologists and nutritionists often emphasize a balanced diet over reliance on supplements.
They suggest that whole foods—rich in vitamins, minerals, and healthy fats—are the best source for hair health.
Foods such as leafy greens, nuts, seeds, fish, and eggs can provide essential nutrients without the added sugars and potential downsides of gummies.
Conclusion:
Fad or Fact?
In conclusion, hair gummies may not be the ultimate solution for hair health, but they can serve as a helpful supplement for those with specific nutritional deficiencies.
They are convenient and may improve the overall appearance of hair for some users. However, it’s crucial to approach them with realistic expectations and prioritize a balanced diet rich in whole foods.
If you’re considering adding hair gummies to your routine, consult with a healthcare provider or nutritionist to ensure you’re making an informed decision that aligns with your health goals.
FAQs
1. Can hair gummies replace a balanced diet?
No, hair gummies are supplements and should not replace a balanced diet. They can help fill nutritional gaps but should be taken alongside a healthy eating plan.
2. How long does it take to see results from hair gummies?
Results vary, but users may start noticing improvements in hair texture and appearance after 4-12 weeks of consistent use.
3. Are hair gummies safe for everyone?
Most hair gummies are safe for general use; however, individuals with specific health conditions or allergies should consult a healthcare professional before taking them.
4. Can I take hair gummies with other supplements?
Yes, but be cautious of total vitamin and mineral intake to avoid exceeding recommended daily allowances. Consult with a healthcare provider for personalized advice.
5. Are there any side effects of hair gummies?
Some users may experience digestive issues, allergic reactions, or headaches due to high sugar content or specific ingredients. It’s best to start with a small dose to assess tolerance.
References:
Health
Understanding the Spine: Common Conditions and Effective Solutions

Understanding the Spine: Common Conditions and Effective Solutions
The spine is an essential structure in the human body, acting as a central pillar that supports our posture, facilitates movement, and protects the spinal cord.
Despite its importance, many individuals experience various spine-related conditions that can impact their quality of life.
In this comprehensive article, we will explore common spinal conditions, their causes, symptoms, and effective methods to address them.
What is the Spine?
The spine, also known as the vertebral column, is composed of 33 vertebrae arranged in a flexible yet sturdy structure.
It serves several critical functions:
- Support: The spine supports the head and allows for an upright posture.
- Protection: It encases and protects the spinal cord, a crucial component of the central nervous system.
- Mobility: The spine allows for a wide range of movements, including bending, twisting, and turning.
- Weight Distribution: It helps distribute weight and absorbs shock during activities like walking or running.
Understanding the structure and function of the spine is vital for recognizing and addressing the conditions that can affect it.
Common Spinal Conditions
Several conditions can adversely impact the spine, leading to pain, discomfort, and reduced mobility. Here are some of the most common spinal conditions:
1. Herniated Discs
A herniated disc occurs when the soft inner material of a spinal disc bulges out through a tear in the outer layer. This can compress nearby nerves, leading to pain, numbness, or weakness in the arms or legs.
Causes:
- Age-related degeneration
- Heavy lifting or sudden movements
- Trauma or injury
Symptoms:
- Localized back pain
- Radiating pain to the limbs
- Numbness or tingling
Treatment:
- Physical therapy
- Pain management through medications
- In severe cases, surgery may be required.
2. Spinal Stenosis
Spinal stenosis is the narrowing of the spinal canal, which can lead to pressure on the spinal cord and nerves. This condition often occurs in the cervical (neck) or lumbar (lower back) regions.
Causes:
- Age-related changes in the spine
- Osteoarthritis
- Herniated discs
Symptoms:
- Pain or cramping in the legs
- Weakness or numbness
- Difficulty walking or standing for extended periods
Treatment:
- Physical therapy and exercise
- Medications for pain relief
- In some cases, surgical decompression may be necessary.
3. Scoliosis
Scoliosis is an abnormal curvature of the spine, often appearing in childhood or adolescence. While many cases are mild, severe scoliosis can lead to complications.
Causes:
- Idiopathic (unknown cause)
- Congenital (present at birth)
- Neuromuscular conditions
Symptoms:
- Uneven shoulders or hips
- Visible curvature of the spine
- Back pain
Treatment:
- Monitoring and observation for mild cases
- Bracing for growing children
- Surgery for severe curvatures.
4. Osteoporosis
Osteoporosis is a condition characterized by weakened bones, making them more susceptible to fractures. This is particularly concerning for the vertebrae, which can lead to compression fractures.
Causes:
- Aging
- Hormonal changes
- Lack of calcium and vitamin D
Symptoms:
- Height loss
- Back pain due to fractures
- A stooped posture
Treatment:
- Medications to strengthen bones
- Nutritional supplements (calcium and vitamin D)
- Weight-bearing exercises to improve bone density.
5. Degenerative Disc Disease
Degenerative disc disease refers to the wear and tear of spinal discs over time, leading to pain and reduced flexibility.
Causes:
- Age-related degeneration
- Repetitive stress on the spine
- Genetics
Symptoms:
- Chronic back pain
- Pain that worsens with movement
- Possible radiating pain in the limbs
Treatment:
- Physical therapy and exercise
- Pain management strategies
- Surgical options for severe cases.
Preventing Spinal Conditions
While some spinal conditions are unavoidable due to genetics or aging, many can be prevented or mitigated through healthy lifestyle choices.
Here are some preventative measures:
1. Maintain Good Posture
Proper posture helps reduce strain on the spine. When sitting, keep your back straight, shoulders relaxed, and feet flat on the ground. When standing, distribute your weight evenly on both feet.
2. Stay Active
Regular physical activity strengthens the muscles that support the spine and improves flexibility. Aim for a balanced routine that includes strength training, aerobic exercise, and stretching.
3. Ergonomic Work Environment
If you spend long hours at a desk, ensure your workspace is ergonomically designed. Adjust your chair, desk height, and computer monitor to reduce strain on your back and neck.
4. Healthy Weight Management
Maintaining a healthy weight reduces stress on the spine and helps prevent conditions like degenerative disc disease and spinal stenosis.
5. Avoid Smoking
Smoking impairs blood flow and can lead to spinal degeneration. Quitting smoking can improve overall health and reduce the risk of spinal issues.
Effective Treatments for Spinal Conditions
If you experience spine-related pain or discomfort, it’s essential to consult a healthcare professional for a proper diagnosis and treatment plan.
Here are some common treatment options:
1. Physical Therapy
Physical therapists develop personalized exercise programs to strengthen the back muscles, improve flexibility, and alleviate pain. They may also use techniques like ultrasound or electrical stimulation to manage discomfort.
2. Medications
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage mild to moderate pain. Prescription medications may be necessary for more severe pain or inflammation.
3. Injections
Corticosteroid injections can reduce inflammation and provide temporary relief for conditions like herniated discs or spinal stenosis. These are typically used when other treatments have failed.
4. Surgery
In severe cases, surgery may be necessary to relieve pressure on the spinal cord or nerves. Common surgical procedures include discectomy (removal of herniated disc material), spinal fusion, and laminectomy (removal of part of the vertebra).
5. Alternative Therapies
Complementary treatments like acupuncture, chiropractic care, and massage therapy may provide relief for some individuals. Always consult with a healthcare professional before trying alternative therapies.
Conclusion
Understanding the spine and its common conditions is crucial for maintaining a healthy lifestyle and preventing potential issues.
By recognizing symptoms early and seeking appropriate treatment, individuals can address spinal conditions effectively.
Implementing preventative measures, such as maintaining good posture and staying active, can significantly reduce the risk of developing spine-related issues.
Prioritize your spinal health, consult with professionals when necessary, and take proactive steps to ensure a healthy and pain-free back.
FAQs
1. What are the common symptoms of spinal conditions?
Common symptoms include localized back pain, radiating pain in the limbs, numbness, tingling sensations, and difficulty with movement.
2. How can I improve my posture while working?
To improve your posture at work, adjust your chair and desk height, use a supportive chair, and ensure your computer screen is at eye level.
3. Can physical therapy help with spinal conditions?
Yes, physical therapy can help strengthen back muscles, improve flexibility, and alleviate pain associated with various spinal conditions.
4. When should I see a doctor for back pain?
If you experience persistent back pain that does not improve with rest, is accompanied by numbness or weakness, or interferes with daily activities, it’s essential to see a doctor.
5. Are there lifestyle changes I can make to prevent spinal issues?
Yes, maintaining a healthy weight, staying active, practicing good posture, and avoiding smoking can help prevent spinal conditions.
References:
Health
Understanding the Causes of Premature Menopause in Women
-

 Trending Stories1 year ago
Trending Stories1 year agoCDC: 1 in 4 Americans Still COVID-Free by End of 2022
-

 Health5 years ago
Health5 years agoMeghan Trainor Shares Motivational New Song ‘Blink’
-

 Health6 months ago
Health6 months agoHow Do Pawpaw Seeds Support Cardiovascular Health?
-

 Health2 years ago
Health2 years agoHow Long Does Monkey Pox Last Before It Surfaces in the Body?
-

 Health3 years ago
Health3 years agoWhat Causes Swollen Body? Understanding Edema and its Triggers
-
 Health3 years ago
Health3 years agoNutrition and the Importance of a Fitness Program – 3 Things to Know
-
 Health3 years ago
Health3 years ago5 Weird Reasons Why Pimples Disappear After Marriage
-

 Health2 years ago
Health2 years agoHealth Benefits Of Pawpaw Seed? 7 Things To Know