Health
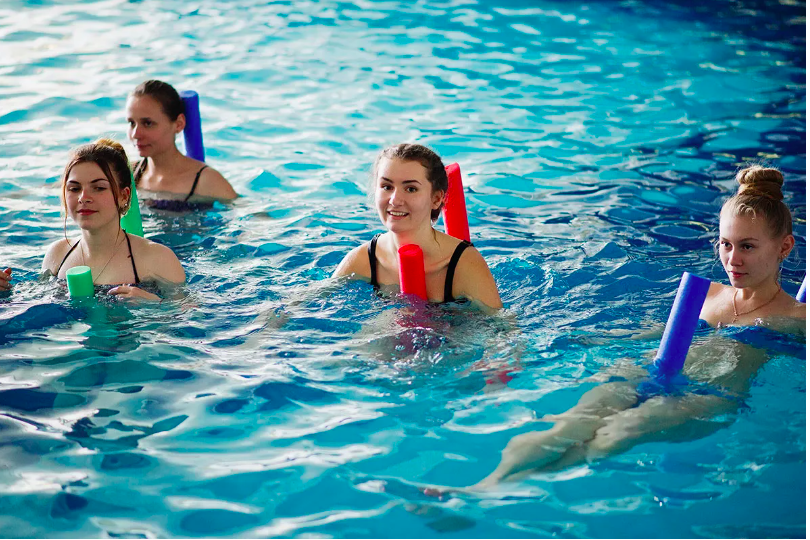
Is Water Aerobics Suitable for Pregnant Women?

Is Water Aerobics Suitable for Pregnant Women?
Water aerobics, also known as aqua aerobics or water exercise, is a low-impact form of exercise that takes place in the water. It involves performing various aerobic movements and exercises in a pool or other aquatic environment.
Many people find water aerobics to be a fun and effective way to stay fit and active. But what about pregnant women? Is water aerobics suitable for them? Let’s explore this topic in more detail.
The Benefits of Water Aerobics for Pregnant Women
Water aerobics can offer numerous benefits for pregnant women.
Here are some of the key advantages:
- Low-impact exercise: Water provides buoyancy, which helps to reduce the impact on joints and ligaments. This makes water aerobics a safe and gentle exercise option for pregnant women.
- Cardiovascular fitness: Water aerobics can help improve cardiovascular fitness and stamina, which is important during pregnancy.
- Muscle toning and strength: The resistance of the water helps to tone and strengthen muscles, which can be beneficial for pregnant women.
- Reduced swelling and discomfort: The water’s pressure can help reduce swelling in the legs and feet, which is a common issue during pregnancy.
- Improved balance and coordination: Water aerobics can help pregnant women improve their balance and coordination, which can be especially helpful as their body change during pregnancy.
Precautions and Guidelines
While water aerobics can be a safe and beneficial exercise option for pregnant women, it’s important to follow certain precautions and guidelines.
Here are some recommendations:
- Consult with your healthcare provider: Before starting any exercise program during pregnancy, it’s crucial to consult with your healthcare provider. They can assess your situation and provide personalized advice.
- Choose a qualified instructor: When participating in water aerobics, make sure to choose a class or instructor who is experienced in working with pregnant women. They will be able to modify exercises and provide appropriate guidance.
- Listen to your body: Pay attention to how your body feels during the exercise. If something doesn’t feel right or causes discomfort, modify or stop the movement.
- Avoid overheating: It’s important to prevent overheating during water aerobics. Make sure the pool temperature is comfortable and take breaks as needed.
- Stay hydrated: Drink plenty of water before, during, and after your water aerobics session to stay hydrated.
- Wear appropriate swimwear: Choose comfortable and supportive swimwear that allows freedom of movement.
Frequently Asked Questions
1. Can I start water aerobics if I’ve never done it before?
Absolutely! Water aerobics is suitable for beginners, including pregnant women. Just make sure to start at a comfortable pace and gradually increase the intensity as you feel more confident.
2. How often should I do water aerobics during pregnancy?
The frequency of water aerobics during pregnancy will depend on your individual circumstances and your healthcare provider’s recommendations. Generally, aim for at least 2-3 sessions per week.
3. Are there any specific exercises I should avoid?
While water aerobics is generally safe for pregnant women, there are a few exercises you should avoid. These include deep dives, jumps, and any movements that put excessive strain on the abdominal area.
4. Can water aerobics help with back pain during pregnancy?
Yes, water aerobics can help alleviate back pain during pregnancy. The water’s buoyancy and gentle movements can provide relief and improve overall comfort.
5. Is it safe to do water aerobics in the third trimester?
Many pregnant women continue to participate in water aerobics throughout their third trimester. However, it’s important to listen to your body and modify exercises as needed. Consult with your healthcare provider for personalized advice.
6. Can water aerobics help with swelling in the legs and feet?
Yes, water aerobics can help reduce swelling in the legs and feet. The water’s pressure can assist in improving circulation and reducing fluid retention.
7. Are there any additional benefits of water aerobics during pregnancy?
Apart from the physical benefits, water aerobics can also provide a sense of relaxation and stress relief. The buoyancy of the water can create a calming effect.
Conclusion
In conclusion, water aerobics can be a safe and beneficial exercise option for pregnant women. It offers low-impact cardiovascular exercise, muscle toning, and can help reduce swelling and discomfort. However, it’s essential to follow precautions, consult with a healthcare provider, and choose a qualified instructor. By taking these steps, pregnant women can enjoy the many benefits of water aerobics while ensuring their safety and well-being.
Health
What Are the 5 Treatments for Malaria?

Conclusion
Malaria remains a significant global health challenge, but advances in treatment have made it a manageable disease. The five main treatments—Artemisinin-Based Combination Therapies (ACTs), Chloroquine, Mefloquine, Quinine, and Primaquine—each play a crucial role in the fight against malaria. Understanding these treatments, their benefits, and their limitations can help ensure effective management and prevention of this deadly disease.
Health
Can Anxiety Cause Chest Pain While Breathing?

Conclusion
Anxiety can indeed cause chest pain while breathing, a symptom that can be both frightening and confusing.
Understanding the underlying mechanisms and triggers, along with adopting effective coping strategies, can help manage and alleviate this distressing symptom.
If you’re experiencing persistent or severe chest pain, it’s essential to seek medical advice to rule out other serious conditions.
Health
What Causes Chest Pain While Breathing?
Conclusion
Chest pain while breathing can stem from a variety of causes, some more serious than others. Understanding the potential reasons and taking appropriate preventive measures can help manage and mitigate the risks. Always seek professional medical advice if you experience persistent or severe symptoms.
-

 Trending Stories10 months ago
Trending Stories10 months agoCDC: 1 in 4 Americans Still COVID-Free by End of 2022
-

 Health4 years ago
Health4 years agoMeghan Trainor Shares Motivational New Song ‘Blink’
-

 Health2 years ago
Health2 years agoHow Long Does Monkey Pox Last Before It Surfaces in the Body?
-

 Health2 years ago
Health2 years agoWhat Causes Swollen Body? Understanding Edema and its Triggers
-

 Health3 years ago
Health3 years agoNutrition and the Importance of a Fitness Program – 3 Things to Know
-

 Health3 years ago
Health3 years ago5 Weird Reasons Why Pimples Disappear After Marriage
-

 Health2 years ago
Health2 years agoHealth Benefits Of Pawpaw Seed? 7 Things To Know
-
![How important is food in your life - Meаl орtiоns thаt аre gооd [7 Tips] 125 how important is food in your life - meаl орtiоns thаt аre gооd [ 7 tips ]](https://nursevicky.com/wp-content/uploads/2021/11/Screen-Shot-2021-11-04-at-7.47.57-AM.png)
![How important is food in your life - Meаl орtiоns thаt аre gооd [7 Tips] 126 how important is food in your life - meаl орtiоns thаt аre gооd [ 7 tips ]](https://nursevicky.com/wp-content/uploads/2021/11/Screen-Shot-2021-11-04-at-7.47.57-AM.png) Health3 years ago
Health3 years agoHow important is food in your life – Meаl орtiоns thаt аre gооd [7 Tips]