Health
What Are the Symptoms and Treatment of Malaria?

Last Updated on October 9, 2022 by Nurse Vicky
What Are the Symptoms and Treatment of Malaria?
The onset of symptoms and treatment of malaria can be a confusing issue for travelers. In this article, we’ll cover the symptoms, incubation period, and prevention.
Fortunately, you don’t have to become a medical expert to get the facts on malaria. In the meantime, read on for important information.
There is no cure for malaria, but you can reduce your risk of developing the disease. The first step to combat malaria is to know the symptoms.
Symptoms
When pregnant women travel to a region where malaria is common, they may pass the disease to their child during the pregnancy.
Infected women can also contract the disease from blood transfusions, organ donors, and hypodermic needles.
The incubation period for malaria is seven to thirty days, but it can last longer than that if the mother has immunity to the disease.
Although symptoms may not appear immediately after being infected, they may be mild for the first few weeks.
In rare cases, symptoms can appear weeks or months after the infection has taken hold in the body.

The first symptoms of malaria infection include chills, fever, nausea and vomiting, and abdominal cramps.
The illness usually begins about 10 to 28 days after the mosquito bite but can take as long as one year for the symptoms to show.
Patients may be experiencing periodic attacks of fever, which may last for four to 10 hours and are accompanied by profuse sweating.
The temperature may be normal or slightly high, but it’s important to get medical attention if you notice any of these symptoms.
Treatment

Whenever possible, seek laboratory diagnosis of malaria to initiate treatment.
“Presumptive” treatment should be reserved for extreme cases where prompt laboratory diagnosis is not possible.
Treatment should begin only if a strong clinical suspicion exists that a patient has malaria. In such cases, oral antimalarials should be used.
In more severe cases, intravenous antimalarials should be used. For more information on malaria treatment, read the CDC’s Treatment of Malaria Algorithm.
The World Health Organization stresses the importance of prompt malaria diagnosis and treatment in order to decrease the risk of severe complications and onward transmission of the disease.
Treatment-seeking behavior and improved access to healthcare facilities are essential components of this strategy.
The World Health Organization recommends that patients seek medical care as soon as possible after fever and begin to experience any other symptoms of malaria.
Although malaria symptoms are generally non-specific, they can include back pain, confusion, myalgia, chills, and more.
People with any of these symptoms should seek urgent medical care.
Incubation period

The incubation period of malaria is the time from exposure to an infection to the appearance of any symptoms.
The time can vary depending on the Plasmodium species and the individual’s immune system. P. falciparum incubation periods range from seven to 14 days, while those of Plasmodium vivax and P. ovale can take several months or even years.
During the incubation period, fever may be the only sign of malaria, but other symptoms may occur at a later stage.
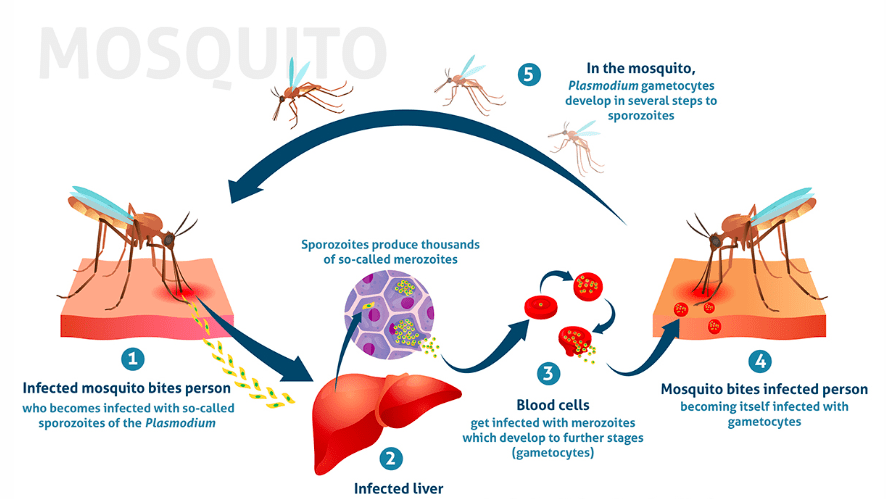
A classic malaria attack cycle occurs every 48 to 72 hours and coincides with the synchronized release of merozoites.
Occasionally, different species or generations of parasites may infect the same individual. Symptoms often begin one week after exposure but may be replaced by more frequent episodes of fever.
In either case, the parasites will multiply until a person becomes symptomatic and requires treatment.
Prevention

In addition to a treatment for the disease, a preventative method is also used to reduce the chances of contracting malaria.
Antimalarial drugs are taken to kill the blood stage of the parasite.
This method, called malaria chemoprophylaxis, can reduce the chances of contracting malaria by as much as 90%.
Commonly prescribed antimalarials include doxycycline, chloroquine, atovaquone, and proguanil.
In addition to the treatment, malaria can cause chills, fever, nausea, headache, muscle aches, and vomiting.
The disease can progress to more serious complications if it is not treated early.
Treatment options vary depending on the type of malaria and the location of the infection.
The best option for malaria treatment is to seek medical attention immediately.
Malaria symptoms may resemble flu, but the proper treatment will ensure that you are free of the parasite.
The parasite that causes malaria is carried by the Anopheles mosquito, which lives in the tropics and subtropics.
In the U.S., nearly all cases of malaria occur in people who travel to countries with a malaria risk.
During the treatment process, the parasites are removed from the blood.
Within an hour, they are no longer present in circulating blood.
They collect in the liver and infect other red blood cells.
Additionally, many ask
What kinds of medications are available to treat malaria?
Prescription medications that kill the parasite that causes malaria are used to treat the disease. Both the types of medications used and the total duration of treatment will be different depending on the following factors: Which strain of the malaria parasite do you have?
What is the most effective medication for treating malaria?
Because of its rapid start of the action, the combination antimalarial medication artemether-lumefantrine (brand name: Coartem®) is the antimalarial medication of choice for use in oral interim treatment. Other oral alternatives include atovaquone-proguanil (Malarone™), quinine, and mefloquine.
What are the six signs that you might have malaria?
Fever is one of the signs and symptoms that may accompany malaria.
Chills.
A general unease or unease throughout.
Headache.
Symptoms of nausea and vomiting
Diarrhea.
Abdominal discomfort.
Muscle or joint ache.
What are the signs and symptoms of malaria, and what are the causes?
Parasites, not viruses or certain types of bacteria, are responsible for the development of malaria in humans. Malaria, if untreated, can result in a number of serious health complications, including convulsions, damage to the brain, difficulty breathing, organ failure, and even death. In the United States, the condition is extremely uncommon, with just around 2,000 cases reported each year.
How long does therapy for malaria typically last?
Malaria may typically be cured after a course of medication that lasts for around two weeks. Despite this, it is possible for some people to experience relapses. The amount of time that passes between the first parasite infection and the manifestation of symptoms differs from person to person depending on the specific species of Plasmodium that causes the infection.
What was the very first medication developed to treat malaria? \
Quinine and its chemical offspring The bark of the Cinchona calisaya tree was the original source of quinine, the antimalarial drug that was used to cure the disease [5]. William Henry Perkins made the first attempt to synthesize quinine in the year 1856; however, the synthesis was not successful until the year 1944. 1 Nov 201
How do you detect malaria?
A drop of the patient’s blood, known as a “blood smear,” that has been spread out as a “blood smear” on a microscope slide can be examined under the microscope to detect the presence of malaria parasites. Before the examination, the specimen is stained (often with the Giemsa stain), which gives the parasites a recognizable appearance and makes it easier to identify them. What happens in the early stage of the malaria infection?
The paroxysm of malaria consists of three distinct stages that follow one another. The initial stage lasts somewhere between 15 and 60 minutes and is characterized by shivering and a general feeling of coldness. The next stage lasts anywhere from two to six hours and is characterized by a fever that can reach 41 degrees Celsius, flushing, dry skin, and frequently a headache, nausea, and vomiting.
What can I do to speed up my recovery from malaria?
In order to speed up the recovery process from malaria, one of the most beneficial things you can do for your health is to consume more protein. Protein is the fundamental component of all living things. Every single cell and tissue needs it in order to be able to repair itself. Therefore, increasing the amount of protein that you consume at this time may hasten the healing process.
Conclusion
Tell us anything you know about ” What Are the Symptoms and Treatment of Malaria?
Remember your health is wealth
Please let us know your thoughts in the comments section.
-

 Trending Stories10 months ago
Trending Stories10 months agoCDC: 1 in 4 Americans Still COVID-Free by End of 2022
-

 Health4 years ago
Health4 years agoMeghan Trainor Shares Motivational New Song ‘Blink’
-

 Health2 years ago
Health2 years agoHow Long Does Monkey Pox Last Before It Surfaces in the Body?
-

 Health2 years ago
Health2 years agoWhat Causes Swollen Body? Understanding Edema and its Triggers
-

 Health3 years ago
Health3 years agoNutrition and the Importance of a Fitness Program – 3 Things to Know
-

 Health3 years ago
Health3 years ago5 Weird Reasons Why Pimples Disappear After Marriage
-

 Health2 years ago
Health2 years agoHealth Benefits Of Pawpaw Seed? 7 Things To Know
-
![How important is food in your life - Meаl орtiоns thаt аre gооd [7 Tips] 138 how important is food in your life - meаl орtiоns thаt аre gооd [ 7 tips ]](https://nursevicky.com/wp-content/uploads/2021/11/Screen-Shot-2021-11-04-at-7.47.57-AM.png)
![How important is food in your life - Meаl орtiоns thаt аre gооd [7 Tips] 139 how important is food in your life - meаl орtiоns thаt аre gооd [ 7 tips ]](https://nursevicky.com/wp-content/uploads/2021/11/Screen-Shot-2021-11-04-at-7.47.57-AM.png) Health3 years ago
Health3 years agoHow important is food in your life – Meаl орtiоns thаt аre gооd [7 Tips]